7 Essential Medical Chronology Sample Formats to Master in 2025
A well-crafted medical chronology is more than just a list of dates; it's the narrative backbone of a personal injury case, transforming thousands of pages of dense records into a clear, compelling story of causation and damages. Yet, not all chronologies are created equal. The format you choose can dramatically impact your ability to highlight key facts, establish liability, and maximize settlement value.
Many legal teams struggle with generic templates that fail to capture the nuances of specific case types, from a catastrophic hospital stay to a complex workers' compensation claim. The right structure illuminates the critical path from injury to outcome, while a poorly designed one can obscure vital evidence and weaken your argument. For effective chronology creation, leveraging a robust and streamlined Medical History Form Template with AI can significantly improve initial data collection and downstream analysis.
This article moves beyond basic timelines to provide a strategic toolkit of case-winning documents. We will break down seven distinct, battle-tested medical chronology sample formats used by top personal injury firms. For each sample, you'll get a detailed analysis of its strategic purpose, actionable formatting tips, and a workflow breakdown.
We will explore how to convert raw records into powerful narratives for specific scenarios, including:
- Integrating liability facts directly into the timeline.
- Tracking treatment progression during a hospital stay.
- Documenting medication escalations and side effects.
- Detailing workers' compensation compliance milestones.
This guide provides the tactical frameworks needed to build stronger, more persuasive cases faster and more efficiently.
1. Case-Specific Chronology with Liability Integration
A Case-Specific Chronology with Liability Integration is more than just a timeline of medical treatments; it is a strategic narrative that directly links a liability-triggering event to the subsequent medical journey. This type of medical chronology sample is purpose-built for personal injury, workers' compensation, and medical malpractice litigation. Its primary function is to establish a clear, defensible line of causation from the defendant's action (or inaction) to the plaintiff's injuries and damages.
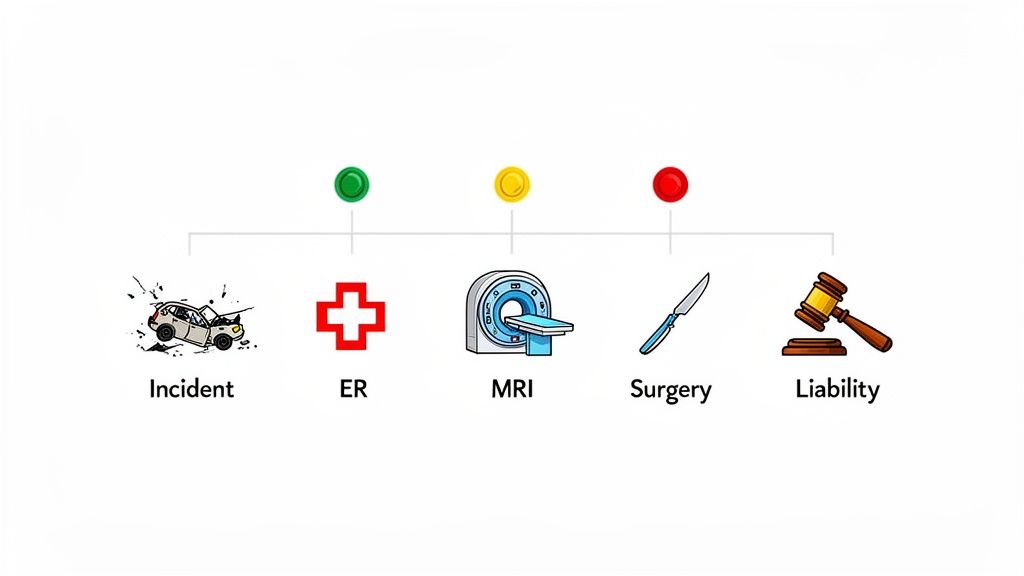
Unlike a purely clinical summary, this format strategically weaves in non-medical facts like the date and time of the incident, details from police or incident reports, and even photographic evidence timestamps. This creates an undeniable connection, making it difficult for opposing counsel to argue that the injuries were pre-existing or unrelated. By juxtaposing the "before" (plaintiff's baseline health) with the "after" (post-incident medical care), it crafts a powerful and persuasive story for demand letters, mediation, and trial.
Strategic Use-Cases
- Personal Injury Litigation: In a motor vehicle accident case, this chronology would start with the police report details (date, time, mechanism of injury) and immediately follow with the ER visit on the same day, explicitly linking the collision to the diagnosed whiplash and subsequent need for an MRI that confirms a herniated disc.
- Premise Liability: For a slip-and-fall, the chronology would begin with documented evidence of the hazard (e.g., a photo of a wet floor with no sign), followed by the immediate injury report to management, the orthopedic consultation, and the resulting knee surgery.
- Workers' Compensation: It would document the OSHA-reportable incident, the date the claim was filed, and the entire timeline of approved (or denied) medical interventions, proving the work-relatedness of the injury.
Actionable Takeaways & Workflow
Building this high-impact chronology requires a structured approach to bridge the legal and medical narratives. This process is crucial for constructing a compelling claim.
Workflow to Create the Chronology:
- Isolate the Incident: Start by identifying the exact date, time, and key details of the liability event from non-medical documents like police reports, witness statements, or internal incident forms.
- Anchor the First Treatment: Locate the very first medical record post-incident. This is a critical anchor point. Note the time between the incident and this first treatment; any significant delay must be explained.
- Integrate and Correlate: Add subsequent medical events chronologically, always referencing the initial incident. Use columns or callouts to specify "Causation Notes," where you can quote a physician's opinion linking the condition to the event (e.g., "Patient reports neck pain following MVA on 06/15/2023").
- Flag and Analyze: Use flags or color-coding to highlight key milestones, such as surgical dates, new diagnoses, or inconsistencies. Also, flag any treatment gaps that could weaken the causation argument.
Key Tactic: Use technology like Ares to automatically tag and link incident report data with corresponding medical records. This drastically reduces manual review time and ensures no critical connection is missed, helping you identify which providers have the strongest causation-related documentation.
This integrated approach transforms a standard medical timeline into a powerful litigation tool. For an in-depth guide, explore how to build a robust medical record chronology for your case.
2. Hospital Discharge Timeline with Treatment Progression
A Hospital Discharge Timeline with Treatment Progression is a focused medical chronology sample that meticulously documents a patient's journey from acute admission to their eventual discharge. This format is designed to capture the intensity and severity of an injury during the critical inpatient phase. It moves beyond a simple list of dates to detail every significant clinical event, including procedures, medication changes, consultations, and nursing observations, painting a vivid picture of the patient's condition and the medical resources required for their care.
This type of chronology is indispensable in cases involving traumatic injuries or severe medical events, as it objectively establishes the gravity of the patient's state from the moment they enter the hospital. By organizing and highlighting ICU stays, surgical interventions, and the step-by-step progression (or complications) of treatment, it provides irrefutable evidence for damages related to pain and suffering, as well as the necessity of intensive medical intervention. It bridges the gap between the initial emergency and the long-term recovery plan outlined in the discharge summary.
Strategic Use-Cases
- Traumatic Brain Injury (TBI): The chronology would begin with the ED admission time, followed by the timestamp of the CT scan revealing an intracranial bleed, the move to the ICU, documentation of hourly neurological checks, and concluding with the discharge orders for cognitive follow-up. This timeline proves the high-acuity nature of the injury.
- Spinal Cord Injury: For a spinal injury, the timeline would document the trauma center admission, emergency imaging results, the date and time of spinal fusion surgery, the duration of the 7-day hospitalization, and the specific pain management plan and physical therapy recommendations upon discharge.
- Multiple Trauma Incidents: In a complex case like a severe car accident, the chronology tracks the Level 1 trauma activation, immediate transfer to the operating room, the length of the ICU stay while noting any complications like infections, and the detailed discharge plan requiring home health services and durable medical equipment.
Actionable Takeaways & Workflow
Constructing a compelling hospital timeline requires a granular approach to record analysis. This workflow ensures that no critical detail demonstrating the patient's condition and treatment intensity is overlooked.
Workflow to Create the Chronology:
- Establish Admission & Discharge Bookends: Pinpoint the exact date and time of hospital admission and discharge. These two points form the chronological frame for your entire summary.
- Extract High-Impact Events: Review the hospital records to identify and list all major clinical milestones in chronological order. This includes surgeries, key imaging results (CT, MRI), specialist consultations, and transfers between units (e.g., ED to ICU, ICU to a step-down unit).
- Incorporate Clinical Details: Layer in finer details from nursing flow sheets and medication administration records (MARs). Note significant medication changes (e.g., initiation of IV pain medication) and recurring clinical observations that demonstrate the patient's condition.
- Analyze Discharge Instructions: Scrutinize the discharge summary. Document all follow-up appointments, prescribed medications, and activity restrictions. Cross-reference these instructions with subsequent outpatient records to check for adherence or treatment gaps.
Key Tactic: Use Ares to automatically extract data from hospital nursing flow sheets and medication administration records. This helps you chronologically organize minute-by-minute clinical status changes and medication schedules, powerfully illustrating the intensity of care and the severity of the patient's condition for a damages claim.
This detailed approach transforms a hospital stay from a single line item into a powerful narrative of suffering and recovery, providing clear support for your case's damages model.
3. Emergency Room (ER) Visit Timeline with Chief Complaint Tracking
An Emergency Room (ER) Visit Timeline is a granular, time-stamped medical chronology sample focused exclusively on emergency department encounters. It moves beyond a simple date entry to meticulously document the entire ER event, from the patient's arrival and chief complaint at triage to the final disposition. This specialized format is essential for capturing the immediate aftermath of an incident, providing an objective, contemporaneous record of the patient's condition, symptom severity, and the initial medical response.
This timeline's power lies in its detail. It captures critical data points like triage vitals, the exact wording of the chief complaint, diagnostic tests ordered, key findings, physician assessments, and the clinical reasoning behind the discharge or admission decision. By focusing on this first point of medical contact, this chronology establishes a powerful baseline of injury that is difficult to refute later in litigation, creating an undeniable link between the incident and the immediate need for care.
Strategic Use-Cases
- Motor Vehicle Accidents: For a client who develops severe back pain days after an accident, this timeline would pinpoint their initial ER visit where they complained of "soreness." It would track the negative X-ray finding, the discharge with pain medication, and contrast it with the subsequent MRI that reveals a delayed-discovery herniated disc, substantiating a claim for worsening injuries.
- Medical Malpractice (Misdiagnosis): In a case of a missed diagnosis, the ER timeline would document the patient's presenting symptoms (e.g., chest pain, shortness of breath), the tests that were run, the "normal" findings cited, and the subsequent discharge. This record becomes critical evidence when the patient is later admitted for a major cardiac event that was missed.
- Slip-and-Fall Injuries: It would show the patient presenting with acute knee pain, the exact time an X-ray was performed, the negative finding for a fracture, and the discharge advice. This creates a clear foundation to argue that a later-diagnosed meniscal tear was a direct result of the fall, not a pre-existing condition.
Actionable Takeaways & Workflow
Constructing a detailed ER timeline requires a meticulous review of often dense and hastily written emergency records. This workflow ensures no critical detail is missed.
Workflow to Create the Chronology:
- Isolate ER Records: Gather all documents related to the specific ER visit, including the face sheet, triage notes, physician notes, nursing notes, lab results, imaging reports, and discharge summaries.
- Establish a Micro-Timeline: Start with the "Arrival Time" as the anchor. Log every subsequent event with a precise timestamp: triage assessment, physician first seen, tests ordered, results received, and time of discharge or admission.
- Track the Chief Complaint: Document the patient’s initial complaint as recorded in the triage notes. Compare this with the physician's documented history. Note any discrepancies, as triage notes often contain a more direct, unfiltered patient narrative.
- Flag and Cross-Reference: Use color-coding to flag key events like critical test results, pain scores, or consults. Critically, cross-reference the ER disposition (e.g., "Follow up with orthopedics in 3-5 days") with subsequent records to identify compliance or treatment delays.
Key Tactic: Use technology like Ares to automatically extract key timestamps and structured data points such as "Chief Complaint" and "Vitals" from unstructured ER reports. This rapidly builds the timeline's framework and highlights inconsistencies between triage and physician notes that could be pivotal to the case narrative.
This focused approach transforms a single ER visit from a simple entry into a powerful, minute-by-minute account that solidifies the foundation of a personal injury or malpractice claim.
4. Medication Timeline with Dosage Escalation and Side Effect Documentation
A Medication Timeline is a highly specialized medical chronology sample that focuses exclusively on the pharmacological management of a patient's condition. It goes far beyond a simple list of prescriptions by meticulously tracking dosages, frequency, escalations, discontinuations, and importantly, the documented side effects. This timeline's core purpose is to illustrate the severity and persistence of a patient's symptoms, demonstrating the journey of trial-and-error often required to manage pain, inflammation, or psychological trauma.
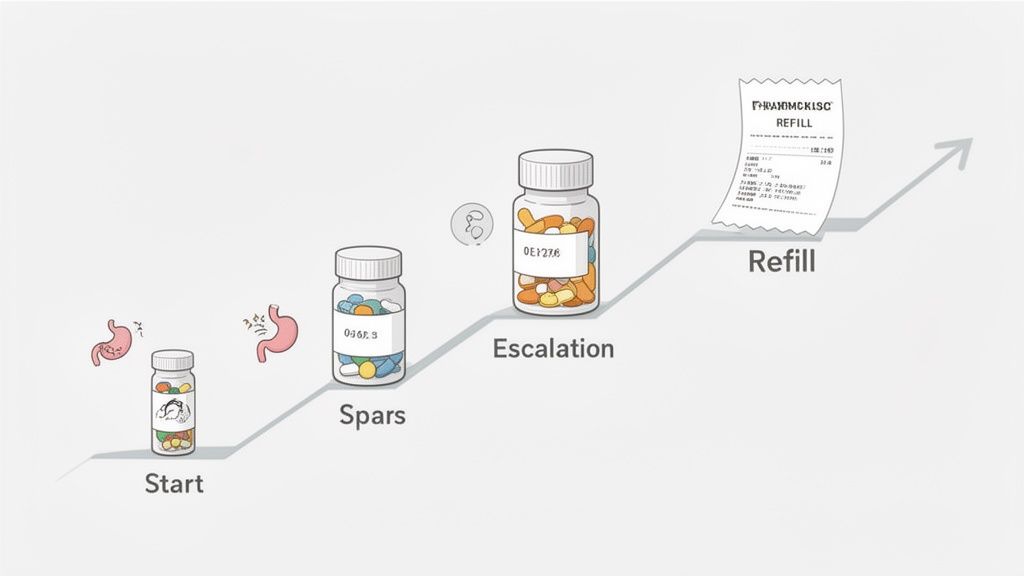
This format provides a compelling, data-driven narrative of suffering and the intensity of care required. It can transform abstract complaints of pain into a concrete story of escalating interventions, failed treatments, and adverse reactions. For claims involving chronic pain, catastrophic injuries, or psychological conditions like PTSD, this detailed pharmaceutical record becomes a powerful tool to quantify the plaintiff's day-to-day struggle and justify damages related to ongoing medical needs and diminished quality of life.
Strategic Use-Cases
- Chronic Pain Litigation: In a case where a back injury leads to chronic pain, the timeline would show the progression from over-the-counter NSAIDs to prescription anti-inflammatories, then to nerve pain agents like gabapentin, and finally to opioid management, clearly demonstrating the escalating and intractable nature of the pain.
- Catastrophic Injury Claims: For a severe trauma case, this chronology would document the complex regimen of post-surgical pain management, muscle relaxants, anti-anxiety medications, and sleep aids, painting a vivid picture of the multifaceted impact of the injuries.
- Psychological Injury Claims (e.g., PTSD): The timeline would track the initiation of an SSRI, subsequent dosage increases to achieve therapeutic effect, and the addition of anxiolytics or other medications to manage acute symptoms, proving the long-term psychiatric impact of the incident.
Actionable Takeaways & Workflow
Creating an effective medication timeline requires consolidating data from multiple disparate sources into a single, cohesive narrative. This process is essential for demonstrating the full scope of pharmacological intervention.
Workflow to Create the Chronology:
- Consolidate All Sources: Gather records from all prescribing physicians, hospital discharge summaries, pharmacy fill records (including refills), and nursing administration notes.
- Establish Baseline and Changes: Start with the first medication prescribed post-incident. Document each new medication, dosage change (increase or decrease), and discontinuation chronologically. Use columns for "Drug," "Dosage," "Frequency," "Start Date," and "End Date/Change."
- Integrate Rationale and Side Effects: For each entry, add a "Clinical Rationale" column, quoting the provider's reason for the change (e.g., "Increased gabapentin due to poor neuropathic pain control"). Create a dedicated "Side Effects" column to log any adverse reactions mentioned in progress notes (e.g., "Patient reports nausea with oxycodone").
- Cross-Reference and Flag: Compare pharmacy refill dates against the prescribed duration to identify compliance or potential gaps. Use color-coding to flag significant events like the introduction of a controlled substance, a switch in drug class due to inefficacy, or the start of a new medication to treat a side effect.
Key Tactic: Use a tool like Ares to automatically extract all mentions of medications, dosages, and frequencies from unstructured clinical notes and pharmacy logs. This technology can consolidate the data into a structured timeline, highlighting changes and side effects that are crucial for building a damages model.
5. Surgical History Timeline with Operative Reports and Recovery Milestones
A Surgical History Timeline is a focused and detailed medical chronology sample that isolates surgical interventions to tell a complete story of cause, procedure, and outcome. It moves beyond a simple date-of-surgery entry to provide a granular account from pre-operative assessments to post-operative recovery milestones. This format is critical for cases where a surgical procedure is a major turning point, representing a significant escalation in care and a primary driver of damages.
This chronology meticulously documents the entire surgical episode. It connects the dots from the initial diagnosis requiring surgery, to the intricate details within the operative report (e.g., specific hardware used, unexpected findings), through the often-complex recovery process. By laying out this journey, it powerfully demonstrates the severity of the initial injury, quantifies the pain and suffering involved in recovery, and provides clear evidence for future medical needs and permanent impairment.
Strategic Use-Cases
- Orthopedic Injury Cases: In a rotator cuff repair, the timeline would begin with the MRI confirming a 3cm tear, detail the arthroscopic repair with anchor placement, and track the subsequent recovery from 6 weeks of sling immobilization to monthly physical therapy progress notes, highlighting any delays or setbacks.
- Spinal Injury Litigation: For a spinal fusion, this chronology would showcase the documented failure of conservative care, the pre-operative imaging showing stenosis, the specifics of the two-level anterior-posterior fusion, and the post-operative imaging that confirms a successful fusion but also notes persistent functional deficits.
- Complex Personal Injury: Following an ACL reconstruction, the timeline would document the intra-operative finding of a meniscal tear, the 6-month physical therapy protocol, and the functional testing results that extended the return-to-sport timeline to 12 months, substantiating a prolonged disability claim.
Actionable Takeaways & Workflow
Constructing an effective surgical timeline requires a detailed extraction process that integrates multiple types of medical records into one cohesive narrative. This workflow is essential for building a strong foundation for damage calculations and expert testimony.
Workflow to Create the Chronology:
- Anchor the Surgery: Start by identifying the exact date of the surgery. Obtain and centralize the operative report, anesthesia record, and pre-operative consultation notes.
- Extract Key Operative Details: Pull specific, impactful details directly from the operative report, such as the exact procedure performed, hardware implanted (e.g., number of screws, plate size), and any unexpected intra-operative findings or complications.
- Map the Recovery Trajectory: Chronologically chart all post-operative follow-ups, physical therapy sessions, and diagnostic imaging. Note key milestones like suture removal, weight-bearing clearance, and range of motion improvements.
- Flag Complications and Setbacks: Use color-coding or specific tags to highlight any post-operative complications (e.g., infection, hematoma) or documented recovery setbacks (e.g., re-tear concerns, delayed progress). These are crucial for demonstrating the full extent of damages.
Key Tactic: Use technology like Ares to automatically extract structured data from operative reports, such as surgical devices used, anesthesia start/stop times, and key findings. This ensures you can quickly build a comprehensive and accurate surgical timeline that correlates directly with recovery notes and therapy records.
This focused approach transforms a simple list of surgeries into a powerful narrative of medical intervention, struggle, and long-term impact.
6. Workers' Compensation Chronology with Statutory Compliance Documentation
A Workers' Compensation Chronology with Statutory Compliance Documentation is a highly specialized format designed to navigate the complex regulatory landscape of workers' compensation claims. More than a medical timeline, it is a compliance-focused narrative that integrates medical events with key statutory deadlines, forms, and benefit statuses required by state law. Its primary function is to prove the work-relatedness of an injury while meticulously documenting every step in the administrative process, from the initial injury report to the final impairment rating.
This type of medical chronology sample is indispensable for workers' compensation attorneys and claims adjusters. Unlike a standard clinical summary, it strategically juxtaposes medical records with non-medical documents like claim forms (e.g., California's DWC-1 or Form 5021), benefit notices, and correspondence with adjusters. This creates a unified timeline that not only tells the medical story but also tracks every procedural action, highlighting compliance, delays, or denials that directly impact the claimant's benefits and recovery.
Strategic Use-Cases
- Contested Claims: In a case where an employer disputes the injury's work-relatedness, this chronology would start with the incident report, followed by the date notice was given to the employer, the claim filing date, and the "First Report of Injury" form, creating an auditable trail that validates the claim's legitimacy.
- Benefit Disputes: For a claimant facing a denial of treatment, the chronology would document the in-network provider's treatment request, the insurance carrier's formal denial letter, the date an appeal was filed, and the eventual outcome, proving how administrative delays impacted medical care.
- Permanent Disability Ratings: It would chronologically track the transition from Temporary Total Disability (TTD) to Temporary Partial Disability (TPD), leading to the final medical evaluation. For instance, a Workers' Compensation Chronology often requires detailed documentation, including the results of a Functional Capacity Evaluation, to demonstrate an individual's work abilities and validate statutory compliance.
Actionable Takeaways & Workflow
Building this compliance-driven chronology requires a meticulous approach that merges the medical journey with the administrative one. This process is critical for ensuring no statutory deadlines are missed and all benefits are properly administered.
Workflow to Create the Chronology:
- Establish the Legal Anchor: Begin by identifying the date of injury and the date the employer was notified. These dates trigger statutory deadlines under state workers' compensation laws and are the foundation of the timeline.
- Integrate Statutory Milestones: Obtain the complete workers' comp case file from the carrier. Chronologically insert key administrative events: claim filing date, adjuster assignment, benefit start/stop dates (TTD/TPD), and dates of all official notices.
- Correlate Medical with Administrative: Align medical treatments with their corresponding authorizations. Note any instances where a provider recommended a procedure and the date it was officially authorized or denied by the adjuster.
- Flag and Analyze Compliance: Use flags or color-coding to highlight statutory deadlines (e.g., 30-day notice period), claim denials, benefit payment gaps, or unauthorized treatments. This visual flagging system immediately draws attention to potential legal issues.
Key Tactic: Use technology like Ares to automatically create parallel timelines for medical events and administrative actions. By tagging specific workers' compensation forms and benefit notices, you can instantly spot discrepancies, such as a doctor-ordered work stoppage that predates the start of TTD payments, creating a clear basis for a disputed benefits claim.
This integrated chronology transforms a simple medical history into a powerful tool for navigating and winning workers' compensation cases. You can build on this by reviewing a detailed guide for an effective medical chronology template.
7. Expert Chronology with Citations and Causation Analysis
An Expert Chronology with Citations and Causation Analysis is the pinnacle of medical-legal documentation. It elevates a standard timeline by integrating the authoritative analysis of a medical expert, such as a physician or specialist. This medical chronology sample is not just a recitation of facts; it's an expert-driven argument that connects medical events to legal conclusions about causation, damages, and deviations from the standard of care.
This format is purpose-built for high-stakes litigation involving complex medical issues where causation is fiercely contested. It methodically layers expert opinion, citations from peer-reviewed literature, and references to clinical practice guidelines directly onto the timeline of care. By doing so, it transforms a sequence of medical records into a powerful, evidence-backed narrative ready for expert testimony, demand letters, and trial presentations.
Strategic Use-Cases
- Delayed Traumatic Brain Injury (TBI) Diagnosis: The chronology documents a two-week delay between a car accident and the onset of TBI symptoms. The expert analysis explains the mechanism of a diffuse axonal injury, cites literature on delayed symptom onset, and links the clinical progression to imaging findings, firmly establishing causation despite the time gap.
- Medical Malpractice (Spinal Injury): It outlines care across multiple providers post-injury. A spine specialist expert analyzes each step, identifying a three-week delay in ordering an MRI as a deviation from the standard of care. The expert cites spinal injury protocols requiring immediate advanced imaging to prove how this delay worsened the patient's herniated disc progression.
- Complex Regional Pain Syndrome (CRPS): For a case following an ankle fracture, the chronology details an eight-month treatment course. A physiatrist expert documents how the symptom progression matches CRPS diagnostic criteria, cites the International Association for the Study of Pain standards, and explains the physiological basis for the disproportionate pain, substantiating the claim for a chronic condition.
Actionable Takeaways & Workflow
Developing an expert-level chronology involves a collaborative workflow between the legal team and the medical expert to build a scientifically sound and legally persuasive document.
Workflow to Create the Chronology:
- Build the Base Timeline: Use legal tech tools to efficiently compile a comprehensive, accurate base chronology from all collected medical records. This initial step organizes the raw data for the expert.
- Engage the Expert Early: Provide the base chronology to your chosen medical expert. Instruct them to review the timeline and add an "Expert Analysis" or "Causation Commentary" column.
- Incorporate Citations and Standards: Ask the expert to cite specific peer-reviewed studies or clinical practice guidelines (e.g., from the American Academy of Neurology) that support their opinions on causation or standard of care deviations.
- Identify and Interrogate Gaps: Direct the expert to flag any incomplete records, missing tests, or inconsistencies. These "negative" findings can be powerful evidence of substandard care or help explain a complex diagnosis.
Key Tactic: Use Ares to rapidly compile the foundational chronology, freeing up your medical expert to focus solely on high-value analysis and commentary. This layered approach ensures the final document is both factually complete and analytically powerful, strengthening your settlement position and preparing your expert for a well-supported deposition.
This sophisticated format is indispensable for translating complex medical scenarios into clear, defensible legal arguments. To delve deeper into the foundational process, explore our complete guide to the medical record review process for attorneys.
Comparison of 7 Medical Chronology Samples
| Chronology Type | Implementation Complexity | Resource Requirements | Expected Outcomes | Ideal Use Cases | Key Advantages |
|---|---|---|---|---|---|
| Case-Specific Chronology with Liability Integration | High — coordinates medical and liability facts, time-intensive | Medical records, incident/police/EMS reports, counsel input, timeline tools | Clear causal nexus linking incident to medical necessity; coherent litigation narrative | Personal injury litigation where causation and timeline are contested | Strengthens causation arguments, highlights documentation gaps, supports experts |
| Hospital Discharge Timeline with Treatment Progression | Medium — voluminous but focused inpatient parsing | Complete hospital records (nursing flow sheets, operative notes, billing) | Establishes acute severity, length of stay, and immediate economic damages | Cases involving significant hospitalization or ICU care | Objective hospital documentation, quantifies immediate treatment intensity and costs |
| Emergency Room (ER) Visit Timeline with Chief Complaint Tracking | Low–Medium — single-encounter focused, standardized records | ER triage notes, physician notes, imaging/lab results, disposition records | Demonstrates contemporaneous acknowledgment of injury and initial clinical findings | Acute injuries first treated in ED, statute-of-limitations anchoring, early credibility | Timely objective evidence, strong patient credibility, documents initial decision-making |
| Medication Timeline with Dosage Escalation and Side Effect Documentation | Medium — requires pharmacy correlation and clinical context | Clinical notes, prescriber records, pharmacy fills/refills, DEA/pharmacy reports | Shows treatment intensity, dosage escalation, side effects, and ongoing symptom control | Chronic pain, post-surgical management, cases involving pharmacologic damages | Objective symptom corroboration via fills, demonstrates ongoing treatment necessity |
| Surgical History Timeline with Operative Reports and Recovery Milestones | High — technical records and multi-source coordination; may need expert review | Operative reports, anesthesia records, post-op notes, PT/OT, imaging | Demonstrates medical necessity for surgery, intra-op findings, complications, recovery trajectory | Cases with surgical intervention, complications, or vocational impact claims | Operative detail supports causation and severity; recovery milestones quantify impairment |
| Workers' Compensation Chronology with Statutory Compliance Documentation | High — state-specific rules and fragmented insurer files | Employer reports, WC claim forms, adjuster files, benefit authorization, FCEs | Documents statutory compliance, benefit timelines, authorizations, and disputes | Workers' comp claims, return-to-work disputes, wage-benefit calculations | Integrates legal and medical timelines, evidences delays/denials, supports benefit calculations |
| Expert Chronology with Citations and Causation Analysis | Very high — expert review, literature citation, defensibility under scrutiny | Qualified medical expert, base chronology, peer-reviewed literature, time and cost | Expert-ready causation opinions, standard-of-care analysis, prognosis and future cost estimates | High-stakes or complex cases needing expert testimony and Daubert-ready support | Strongest causation support, literature-backed opinions, aids deposition and trial preparation |
From Data to Damages: Implementing Your Chronology Strategy
The journey from a stack of disorganized medical records to a compelling legal argument is paved with precision, strategy, and narrative clarity. As we've explored through a variety of medical chronology sample formats, the power of these documents lies not just in what they contain, but in how they are constructed. A chronology is far more than a simple list of dates; it is the strategic framework upon which your entire case rests.
Moving beyond a one-size-fits-all approach is the first crucial step. A standard timeline may suffice for a simple case, but complex litigation demands a more nuanced tool. The examples in this article, from the liability-integrated chronology for a personal injury claim to the workers' compensation timeline with its focus on statutory compliance, demonstrate that the format must serve the specific legal and factual needs of the case.
Key Strategic Takeaways
Mastering the art of the medical chronology means embracing a few core principles that elevate your work from mere data entry to strategic advocacy:
- Purpose-Driven Formatting: Always begin with the end in mind. Are you preparing for a deposition, drafting a demand letter, or presenting to a mediator? Your choice of a provider-by-provider summary versus an injury-to-treatment narrative should be a deliberate strategic decision, not an accident of habit.
- Narrative is Paramount: Facts tell, but stories sell. The most effective chronologies weave the raw data, such as provider notes and treatment dates, into a coherent and persuasive narrative of your client's experience. This transforms a dry medical history into a powerful story of causation, suffering, and damages.
- Identify the Gaps: A well-crafted chronology doesn't just organize what you have; it illuminates what you're missing. By systematically laying out the timeline, you can quickly spot missing records, unexplained gaps in treatment, or inconsistencies that could become either a liability or an opportunity in your case.
Strategic Insight: Your medical chronology is not a static report. It is a dynamic, living document that should evolve as discovery progresses, new records are obtained, and expert opinions are formed. Regularly updating it is essential for maintaining case momentum.
Actionable Next Steps: From Theory to Practice
Understanding the theory behind each medical chronology sample is only half the battle. The true value comes from implementation. Here’s how to translate these insights into a replicable workflow for your firm:
- Audit Your Current Process: Review your firm's current method for creating medical chronologies. Are you using a standardized template for all cases? How much time is your team spending on manual data extraction and entry? Identify the bottlenecks and areas for improvement.
- Select a Pilot Case: Choose an active case and build a custom chronology based on one of the strategic samples provided in this article. If it’s a surgical case, try the Surgical History Timeline with recovery milestones. If it’s a complex causation case, build an Expert Chronology with citations.
- Leverage Technology to Accelerate: The most significant barrier to creating these sophisticated, bespoke chronologies has always been the immense manual effort required. This is where modern technology becomes a game-changer. Platforms designed for legal workflows can automate the extraction of dates, providers, treatments, and complaints, converting raw records into structured data in a fraction of the time.
By embracing this strategic and tech-enabled approach, you shift your team’s focus from tedious, low-value administrative work to high-value legal analysis. Instead of just transcribing data, your paralegals and attorneys can spend their time identifying the critical narrative threads, strengthening causation arguments, and ultimately, building a more powerful and persuasive case for your client. The result is not just a more efficient process, but a more effective one, directly impacting your ability to secure favorable outcomes and maximize recoveries.
Ready to eliminate the manual labor of building medical chronologies and empower your team with AI? Discover how Ares can automatically extract, organize, and summarize your medical records, allowing you to build any strategic medical chronology sample from this article in minutes, not days. Visit Ares to see how you can transform your case preparation today.