Medical Records Review for Attorneys: Streamline Cases and Spot Red Flags

For any personal injury firm, how you handle medical records isn't just an administrative chore—it's the bedrock of your entire case strategy. Get it right, and you’re on the path to a strong settlement. Get it wrong, and you're fighting an uphill battle from day one. Sticking with outdated, manual review processes is one of those silent killers that can slowly drain your firm’s resources and weaken your claims before you even get to the negotiating table.
The Hidden Costs of an Outdated Review Process
Too many PI firms just accept that slogging through medical records is a necessary evil. They see the long hours and tedious work as the cost of doing business. But the truth is, a disorganized, manual review process creates a massive financial and strategic drag that echoes through every single case file. These aren't just small annoyances; they're significant, hidden costs that eat directly into your firm's profitability and, more importantly, your clients' outcomes.
The first wall you hit is the sheer volume of paper. With nearly 400,000 personal injury claims filed each year in the U.S. alone, the mountain of documents is staggering. Think about it: a standard 1,000-page medical file can easily take a paralegal over 15 hours to review manually. At typical billing rates, that’s over $500 per case spent on just one task—time that could be spent advocating for the client or pushing settlement talks forward.
The True Price of Inefficiency
Beyond the direct costs, the real damage from a slow review process shows up in more subtle, harmful ways. When it takes weeks to get through the records, demand letters get delayed. This gives the defense more time to dig in their heels and build their case while your client is left waiting. Worse, it dramatically increases the risk of undervaluing the claim. When your team is buried under thousands of pages, it's easy to miss a crucial note about a future surgery or overlook a detail that speaks to the client's long-term suffering.
This manual grind creates a domino effect of problems:
- Wasted Paralegal Hours: Your best people end up doing clerical work—sifting through duplicate records and organizing files—instead of focusing on high-value tasks like drafting motions, communicating with clients, or preparing for depositions.
- Undervalued Claims: It’s so easy to miss the smoking gun—that one line from a physical therapist about causation or a doctor's note on long-term prognosis. When those details are missed, insurance adjusters pounce, and settlement offers come in low.
- Increased Error Rate: Manual data entry is a recipe for mistakes. A typo in a date or a misinterpretation of a diagnosis can create inconsistencies that undermine the credibility of your entire demand package.
A disorganized review process is like trying to build a house on a shaky foundation. It doesn't matter how brilliant your legal arguments are if the medical facts supporting them are incomplete or wrong.
Navigating Compliance and Security Risks
Let’s not forget the compliance minefield. Every page of a medical record contains protected health information (PHI), and your firm is responsible for keeping it secure. A single breach doesn't just tarnish your reputation; it can bring on staggering fines and legal penalties.
This is why having a secure, systematic approach is non-negotiable. For instance, any system you use must be able to work with HIPAA compliant transcription services to avoid the hidden risks that come with handling sensitive patient data. It's not just about being efficient; it's about protecting your clients and your firm from serious liability. You can dive deeper into this topic in our guide on https://areslegal.ai/blog/hipaa-compliant-document-management.
Moving past these old-school methods isn't just a matter of convenience; it’s a strategic necessity. The table below breaks down the common pain points of manual review and contrasts them with the modern solutions available today.
Manual vs. Modernized Medical Record Review
| Challenge in Manual Review | Impact on the Firm | The Modern Solution |
|---|---|---|
| Time-Consuming & Tedious | Drains paralegal and attorney hours; over 15 hours per 1,000 pages. | AI-powered tools extract key data in minutes, not days. |
| High Potential for Errors | Manual data entry leads to missed facts, typos, and weak narratives. | Automated fact extraction and chronology building ensure accuracy and consistency. |
| Inconsistent Summaries | Different paralegals create summaries with varying quality and focus. | Standardized templates and AI-generated summaries create uniform, high-quality work product. |
| Security & HIPAA Risks | Scattered files and unsecured emails create compliance vulnerabilities. | Centralized, encrypted, and HIPAA-compliant document management systems protect client data. |
| Delayed Case Progression | Slow review leads to late demand letters and stalled negotiations. | Faster turnaround times accelerate the entire case lifecycle, from intake to settlement. |
As you can see, the contrast is stark. Embracing a more modern, tech-assisted workflow isn’t just about saving time—it’s about building stronger cases, securing better outcomes, and protecting your firm from unnecessary risks.
Laying the Groundwork: Your Intake and Organization System
Any seasoned paralegal or attorney will tell you that a medical record review doesn't start when you open the first file. It starts way before that, with a rock-solid, repeatable system for intake and organization. If you don't have a standardized process, you're inviting chaos—lost documents, blown deadlines, and critical mistakes that can hamstring a case before you even get started.
Building this foundation isn't about reinventing the wheel, but it does demand discipline. The entire point is to create a predictable workflow. Every record needs to be requested, received, logged, and stored securely the exact same way, every single time. This consistency takes the guesswork out of the equation and creates a clean, clear audit trail for every piece of paper that comes through your door. It’s the bedrock of your entire case strategy.
The flowchart below drives this point home, showing how quickly the page count spirals into real time and money spent on a case.
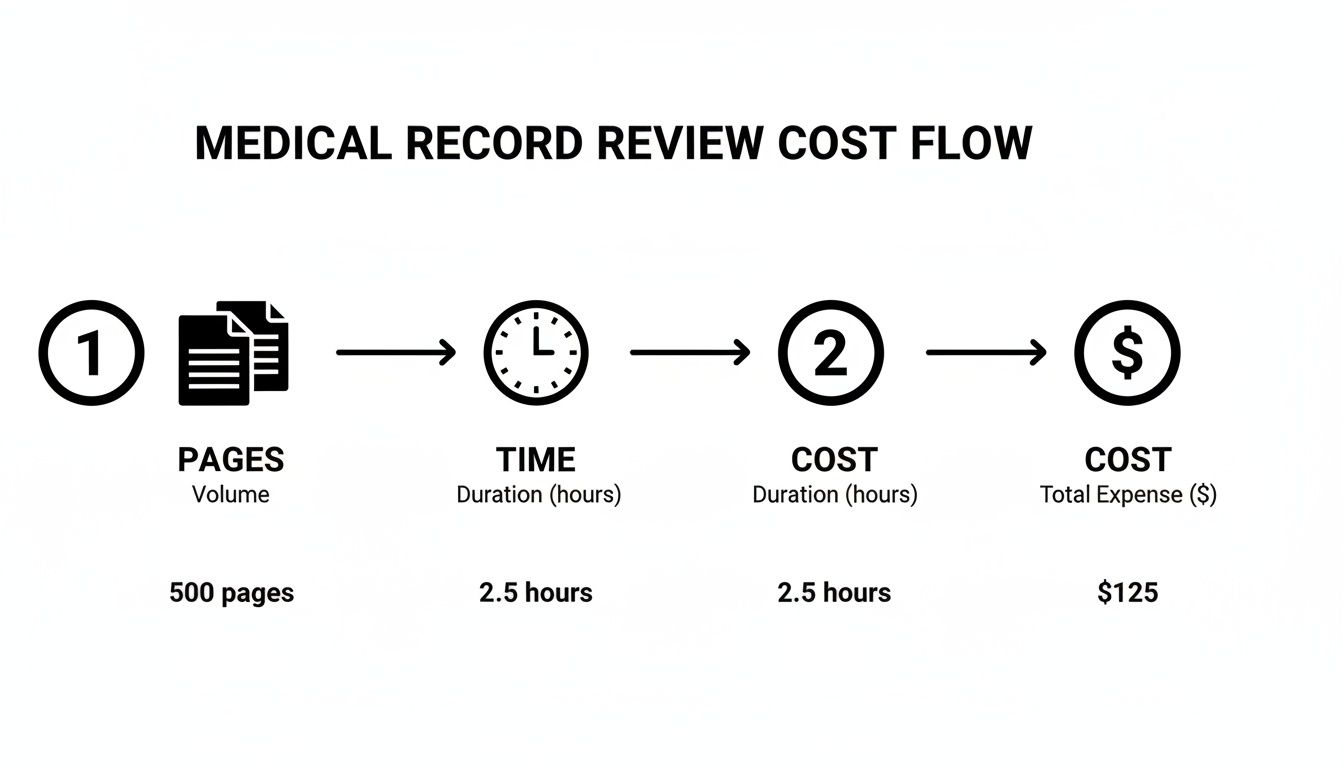
This isn't just a pretty graphic; it's a warning. Small inefficiencies in how you organize and prioritize records don't just waste a few minutes here and there. They compound, snowballing into serious time and cost overruns that can eat into your firm's bottom line.
Mastering Your Digital Filing Cabinet
A bulletproof system is built on meticulous digital file management. In today's world, just dumping PDFs into a generic client folder won't cut it. You need a structured approach that lets anyone on your team find exactly what they need in seconds.
Your first line of defense is a consistent naming convention. It sounds simple, but a logical format makes a night-and-day difference. For example, a file named [ClientLastName]-[ProviderName]-[DateOfService-YYYY-MM-DD].pdf is infinitely more useful than scan_001.pdf.
This one small habit instantly makes your files sortable, giving you an at-a-glance timeline of your client's treatment right from the folder view. For a deeper dive, our guide on how to organize medical records breaks this down even further.
Beyond file names, your storage setup is absolutely critical.
- Centralized Cloud Storage: All case documents must live in a single, secure cloud platform, like your practice management system. This stops files from getting siloed on individual desktops or lost in email threads.
- A Smart Folder Structure: Create a master folder template that you clone for every new case. Think subfolders like
01_Intake,02_Medical Records,03_Correspondence,04_Demand, etc. This creates uniformity across your entire firm. - Strict Access Controls: Use permissions to control who can view, edit, or download sensitive client data. This isn't just good practice; it's essential for protecting your client and your firm.
How to Prioritize Records for Maximum Impact
Once the records start rolling in, the sheer volume can feel like a tidal wave. The secret is knowing that not all documents carry the same weight. You have to learn where to focus first to quickly grasp the core narrative of the case.
I’ve seen junior paralegals get completely bogged down in months of routine physical therapy notes before they've even touched the initial ER report or operative summary. You have to attack the high-impact documents first—they contain the gold.
Here’s a practical battle plan for prioritizing your review:
- The First 48 Hours: Always start with records from the day of the incident and the immediate aftermath. This means the ambulance run sheet, the emergency room report, and the initial admitting physician's notes. These documents lock in the immediate consequences of the injury.
- Surgeries and Hospital Stays: Next, pull the operative reports, anesthesia records, and hospital discharge summaries. These give you the detailed breakdown of major procedures and the official diagnoses established during their stay.
- The Specialist Opinions: Now, hunt down the reports from key specialists—think orthopedic surgeons, neurologists, or pain management physicians. Their assessments are vital for proving long-term prognosis and future medical needs.
- Objective Diagnostic Evidence: Finally, gather the MRI, CT, and X-ray reports. You don't need to read every line; go straight to the "Impressions" section. This is where the radiologist summarizes the definitive findings.
By tackling the records in this order, you build a powerful, foundational understanding of the case in a fraction of the time. You can quickly size up the severity of the injuries, identify the key treating physicians, and spot potential red flags long before you've invested dozens of hours into less critical paperwork. This isn't just about being organized; it's about being strategic.
Analyzing Records to Uncover Case-Defining Insights
With all the records in hand and neatly organized, the real work begins. This is where your team transitions from clerks to strategists, digging deep into the clinical data to find the story that will define your case. A proper medical records review for attorneys is less about data entry and more about investigative journalism—you're looking for the narrative thread that turns a stack of paper into a compelling argument for your client.
It’s a process that demands a keen eye and, frankly, a bit of healthy skepticism. You're not just reading; you’re looking for clues, connections, and contradictions that will either make or break your demand.
Pinpointing the Core Factual Evidence
Every powerful demand letter is built on a foundation of solid, undeniable medical facts. Your first pass through the records should be laser-focused on extracting these core data points. You’re essentially building the skeleton of your case, and precision is everything.
Focus on pulling these key elements:
- Key Dates and Timelines: Log every single significant event. This includes the initial ER visit, every follow-up with a specialist, and each physical therapy session. This timeline becomes the spine of your entire chronology.
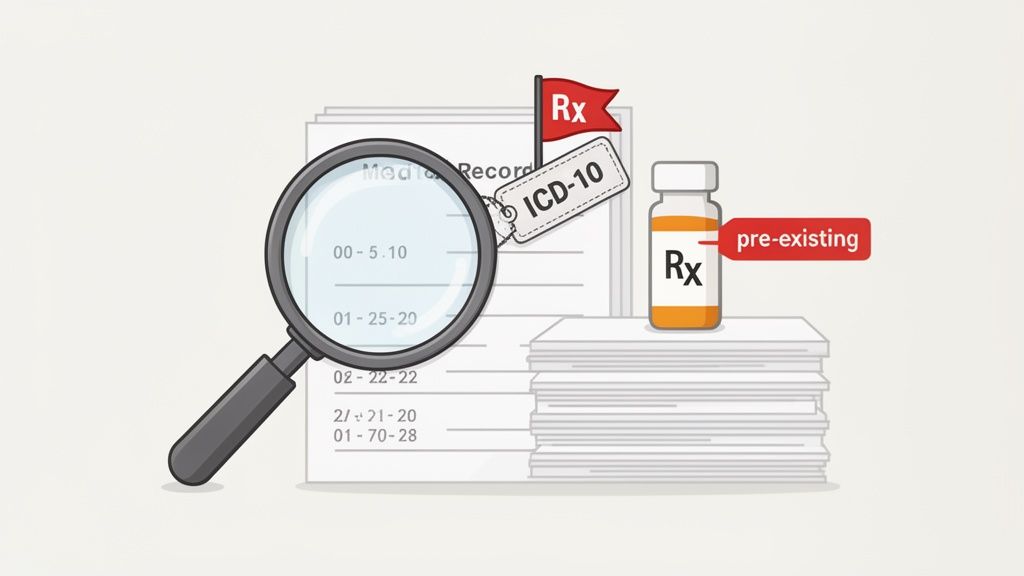
- Official Diagnoses with ICD Codes: Pinpoint every formal diagnosis made by a provider. Pay special attention to the ICD-10 codes—like S52.501A for a displaced radial styloid fracture of the right wrist. These codes aren't just jargon; they are the universal language of medicine and lend objective weight to your client's injuries.
- Specific Treatments and Procedures: Make a detailed list of every medical intervention. This means surgeries (note the CPT codes), physical therapy plans, injections, and medications administered. This evidence proves the extent of care your client needed.
- Prescription Histories: Catalog every single prescription, noting the drug, dosage, and fill dates. This is a powerful, tangible way to demonstrate the severity of your client's pain and suffering.
Think of this stage as an archeological dig. You're carefully unearthing the artifacts of the case. Each diagnosis, prescription, and procedure note is a piece of evidence that helps reconstruct the story of your client's injury and recovery.
Hunting for Red Flags and Defense Ammunition
A truly effective review doesn't just look for the good stuff. It actively hunts for the evidence the defense will use against your client. Finding these red flags early is a massive strategic advantage, giving you time to build a counter-narrative and prepare your client.
You absolutely have to train your team to spot these landmines before the adjuster or opposing counsel does.
Common Red Flags to Watch For
- Mentions of Pre-Existing Conditions: Look for any note, however brief, of a past injury or condition in the same body part. A simple entry about "chronic lower back pain" in the records for a car wreck back injury is a gift to the defense.
- Unexplained Gaps in Treatment: Did your client wait weeks to see a doctor? Is there a month-long gap in their physical therapy visits? The defense will seize on this, arguing the injury wasn't that serious or that something else happened during that gap.
- Notes on Patient Non-Compliance: This is a killer. Look for any mention of missed appointments, failure to follow medical advice, or not doing at-home exercises. The defense will use this to argue your client is to blame for their own slow recovery.
- Inconsistent Subjective Complaints: Watch for conflicting pain ratings. If your client told the ER doc their pain was a 4/10 but later told an orthopedist it was a 9/10, that inconsistency will be used to attack their credibility. Documenting this lets you get ahead of the issue.
- Drug or Alcohol Use: Be on high alert for any mention of alcohol or drug use near the time of the incident. ER toxicology reports or physician notes on substance use history will absolutely be used against your client.
When you find these issues first, you control the story. You can get an expert opinion to distinguish a new injury from an old one, or you can prepare your client to confidently explain a treatment gap in their deposition. This kind of foresight is what separates an average firm from a great one, turning potential liabilities into manageable facts and building a much stronger case.
Crafting Powerful Medical Chronologies and Summaries
Once you have the raw data, the real work begins. A disorganized stack of lab reports and doctor’s notes won’t persuade anyone. Your task is to transform this clinical chaos into powerful legal tools that tell your client's story clearly and convincingly.
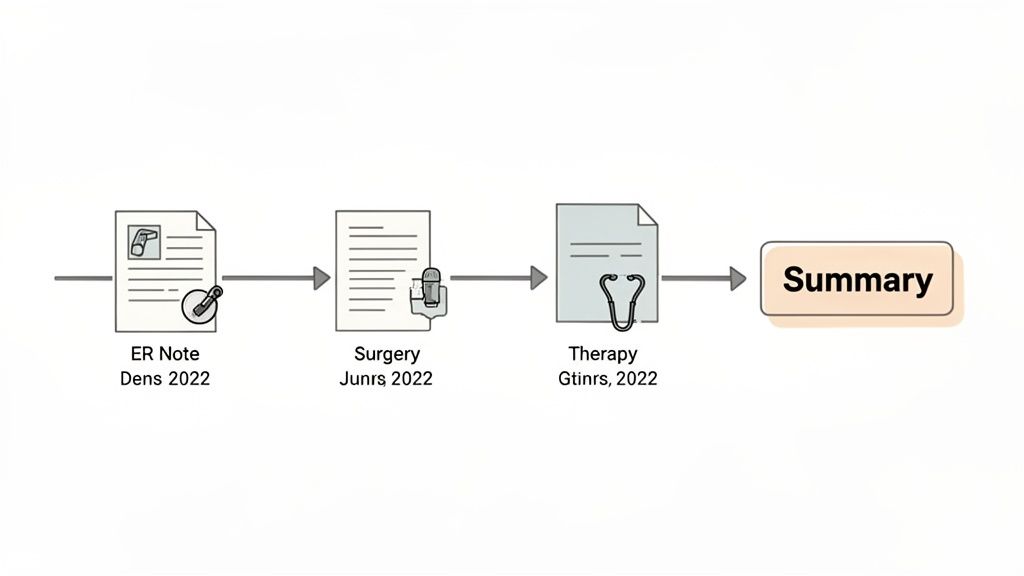
This is where you build the foundation of your case: the medical chronology and the narrative summary. These two documents are closely related but serve very different purposes. Getting both right is fundamental to moving a case toward a great settlement or a successful verdict.
The Medical Chronology: The Factual Timeline
Think of the medical chronology as the undisputed, objective timeline of the case. Its strength comes from its simplicity and factual integrity. This document is not the place for your arguments or interpretations; it's a meticulous, date-driven log of everything that happened to your client from the moment of injury onward.
A rock-solid chronology is essential for proving causation by establishing a clear sequence of events. The industry is moving in this direction, too. In fact, nearly 48% of legal teams now prefer detailed chronologies over high-level overviews because of their depth and clarity.
Your chronology has to be easily scannable and, most importantly, verifiable. Every single entry must be tied directly back to a specific page in the source records. This creates an unimpeachable document that builds trust with both adjusters and opposing counsel.
Here’s a simple, effective structure for your chronology:
- Date of Service: The exact date of the appointment or treatment.
- Provider/Facility: The name of the doctor, clinic, or hospital.
- Event/Treatment Type: A quick description (e.g., "ER Visit," "MRI of Lumbar Spine," "Physical Therapy").
- Key Details & Findings: A concise summary of what happened, including diagnoses, prescriptions, or key test results.
- Source (Bates #): The precise page number where this information can be found.
This layout allows anyone reviewing the file to instantly find and verify the facts, which builds credibility and makes negotiations much smoother.
The Narrative Summary: Weaving a Compelling Story
If the chronology is the skeleton, the narrative summary is the heart and soul of your medical case. Here, you go beyond a simple list of dates to craft a persuasive story. Your goal is to explain the impact of the injuries on your client’s life in a way that truly connects with an adjuster, mediator, or jury.
Unlike the chronology, the summary is topic-driven, not strictly date-based. It synthesizes all that factual information into a cohesive narrative that spotlights the most critical parts of the case.
A great narrative summary connects the dots. It doesn't just say what happened; it explains why it matters—how the diagnosed disc herniation led to debilitating pain, missed work, and the inability to go fishing on the weekends.
To build a powerful narrative, think thematically. I recommend organizing your summary with sections like these:
- Initial Injury and Emergency Care: Set the stage by describing the incident and the immediate medical response.
- Diagnosis and Treatment Course: Walk the reader through the key diagnoses and major medical steps, from surgeries to months of therapy.
- Pain, Suffering, and Lifestyle Impact: This is where you bring the human element to the forefront. Use direct quotes from physician notes or your client’s own words to illustrate the real-world cost of the injury.
- Prognosis and Future Medical Needs: Conclude with the experts' opinions on long-term limitations and why future care is necessary.
This approach transforms dry medical facts into a compelling human story. It gives the case the context and emotional weight that a timeline alone never could, making it an essential tool for your demand package and mediation. A well-crafted summary doesn't just present the evidence; it frames the entire conversation around your client's experience, which is exactly what you need to do to maximize case value.
How AI Is Changing the Game for Medical Record Reviews
The idea of intelligent automation isn't some far-off concept anymore; it's here, and it's already making waves in personal injury law. For as long as anyone can remember, reviewing medical records has been a major bottleneck. It’s a resource-draining slog that slows down case progress and burns out even the most dedicated paralegals.
That whole dynamic is starting to shift, thanks to AI-powered platforms.
Instead of your team spending days or weeks digging through thousands of pages of dense medical jargon, AI tools can get the job done in minutes. This isn't just about speed, either. It’s about a level of detail and accuracy that’s incredibly difficult to sustain manually across a massive case file.
From Days of Work to a Coffee Break
Think about a standard multi-vehicle accident case. You've got records from the ER visit, an orthopedic surgeon, a pain management doctor, and several months of physical therapy. It's not unusual for a file like that to top 1,500 pages. A seasoned paralegal could easily spend 15-20 hours just getting that organized, reviewed, and summarized into a usable chronology.
Now, imagine uploading that same file to an AI platform.
- In just a few minutes, the AI processes and digitizes every single page, even messy handwritten notes.
- It automatically pulls out all the critical data: every diagnosis, treatment, provider, prescription date, and ICD code.
- The system then generates an interactive, hyperlinked medical chronology and a draft narrative summary, ready for review.
What used to be days of tedious manual labor is now finished before you've even finished your coffee. This frees up your legal staff to do what they do best: focus on high-value strategic work like crafting compelling arguments, prepping for depositions, and negotiating better settlements.
The Real-World Impact on Your Firm's Workflow
The efficiency boost is huge. The old way of doing things often saddles PI firms with demand package delays of more than 100 days in 42% of cases. With an AI-assisted approach, firms can save 15+ hours for every 1,000 pages reviewed. More importantly, it improves accuracy in identifying treatment timelines, injury severity, and future medical costs—all critical for calculating damages.
This isn't about replacing paralegals. It's about empowering them. By letting AI handle the repetitive data extraction, you turn your team into high-level analysts who can spot crucial trends and build stronger case narratives from the very beginning.
Automating the initial review also slashes the risk of human error. We’ve all been there. A tired paralegal can easily miss a single critical note on page 847 about a pre-existing condition or a conflicting pain score. AI algorithms don’t get tired. They scan every word with the same sharp focus, flagging subtle patterns and treatment gaps that even a meticulous professional might miss. This is where a top-notch medical record review service built on this technology becomes a real strategic advantage.
Beyond just the review process, keeping up with legal tech is essential. For any attorney trying to navigate this new landscape, understanding the broader implications of AI in law is key to making smart decisions for your practice. By bringing these intelligent systems into your workflow, you can break through old bottlenecks, minimize errors, and ultimately build more powerful, persuasive cases for your clients.
Got Questions? Let’s Talk Medical Records
Even with the best system in place, reviewing medical records can throw some curveballs. Let's tackle some of the most common questions our team gets from personal injury attorneys and paralegals. Getting these answers right can make a huge difference in your firm's efficiency and case outcomes.
What are the biggest mistakes people make during a review?
The classic blunders? Missing records are a big one—failing to get the complete picture from every provider. It's also incredibly easy to gloss over a note about a pre-existing condition or miss a significant gap in treatment when you're staring at a mountain of paperwork.
Another huge, and costly, mistake is spending countless hours manually creating summaries. That’s valuable paralegal time that could be spent on strategy, not just transcription. These slip-ups don't just weaken a case; they can lead to significantly lower settlement offers. A solid checklist helps, but this is where AI-assisted tools really shine. They catch the details a tired human eye might miss across thousands of pages.
How do we make sure our firm stays HIPAA compliant?
HIPAA compliance is non-negotiable. First, you need a secure, encrypted way to receive records, like a dedicated client portal. Standard email is a definite no-go. All your documents should live on encrypted servers or within a legal platform that has top-notch, built-in security.
Internally, you have to lock down access. Not everyone in the firm needs to see every client's sensitive health information, so set strict user permissions. Finally, if you're using any third-party software for medical records review for attorneys, make sure it's explicitly HIPAA compliant and that they'll sign a Business Associate Agreement (BAA). Don't even consider a tool without one. It's about protecting your client, and your firm.
How exactly does AI make medical chronologies more accurate?
Think of it this way: AI doesn't get tired, and it doesn't have biases. It scans every single page to pull out key data—dates, providers, diagnoses, treatments—with relentless consistency. A person doing this manually is bound to make a typo or miss an entry after a few hours of staring at dense records.
AI algorithms are trained to recognize and categorize this information precisely. They can instantly cross-reference a detail on page 5 with something on page 500, spotting connections or inconsistencies you might never notice.
The result is a rock-solid, verifiable medical timeline. It strips out the small human errors that can chip away at your credibility and gives your team a factual foundation they can build a case on with total confidence.
When should we bring in an AI review tool?
The sooner, the better. The best time to use an AI tool is the moment medical records start coming in the door. Uploading documents right at the beginning of the intake process gives you an almost immediate, high-level view of the entire case. This early analysis is a game-changer for strategy.
It means your team can:
- Get a quick read on case viability based on the initial medical evidence.
- Instantly pinpoint which provider records are still missing.
- Spot potential red flags like pre-existing conditions or treatment gaps from day one.
When you bring this technology in at the start, you stop wasting time. Your team can move forward with a clear, data-driven plan instead of waiting weeks just to piece together the full medical story. That proactive approach builds a stronger foundation for everything that follows, from the initial client meeting to the final negotiation.
Ready to stop drowning in paperwork and start building stronger cases faster? Ares is an AI-powered platform that transforms thousands of pages of medical records into clear, actionable insights in minutes.