Mastering the Medical Summary Format for Personal Injury Claims
A good medical summary does more than just list facts from a medical chart. It's a carefully structured document that weaves a patient’s complicated medical history into a clear, chronological story that legal professionals can actually use. For personal injury cases, the gold standard format always includes a few key sections: a case header, a timeline of all encounters, a list of diagnoses, a summary of treatments, a section on functional impact, and an honest look at any gaps in care.
This isn't just about organization; it’s about transforming a mountain of dense records into a persuasive narrative.
Why the Right Format Gives You a Strategic Edge
In the world of personal injury litigation, a well-built medical summary is one of your most powerful tools. It’s not just a document—it’s the story that can make or break a case. When you move beyond a simple list of events, you turn a chaotic stack of medical records into a clear, compelling narrative for adjusters, opposing counsel, and even juries. It becomes a strategic asset, making case reviews faster and shining a spotlight on the critical evidence you need to build a rock-solid claim.
The whole point is to create an objective, easy-to-follow roadmap of your client's medical journey from the moment of injury. This is far more than just listing dates. It’s about connecting the dots between the incident, the treatments, and the real-world impact on your client's life. A messy or incomplete summary can bury the most important facts, weaken your negotiating power, and ultimately sink the value of a claim. On the other hand, a professional summary screams credibility and shows you’ve done your homework from day one.
The Blueprint for Your Medical Argument
Think of your medical summary's format as the architectural blueprint for the medical side of your case. Each section has a specific job, building on the last to paint a complete picture of the client's damages. This logical structure means that anyone picking up the file—from a paralegal in your office to an insurance adjuster on the other side—can quickly understand what happened without getting bogged down in medical jargon.
A logical flow is your best defense against misinterpretation. It forces the reader to focus on the points you want to make. For example, a crisp chronology immediately sets the timeline, while a dedicated "Functional Impact" section translates clinical notes into the real-life consequences that justify damages.
A medical summary isn’t just a shorter version of the records. It's an interpretation that steers the reader toward a specific conclusion. Your format is the framework that makes that guidance clear, logical, and defensible.
To give you a bird's-eye view, here's a quick breakdown of the essential components every effective medical summary needs.
Essential Components of a Personal Injury Medical Summary
This table outlines the core sections of a strong medical summary and explains their role in building your case.
| Component | Purpose in Litigation | Key Information to Include |
|---|---|---|
| Case Header | Provides at-a-glance case identification. | Client name, date of birth, date of incident, claim number, and brief case identifier. |
| Chronology of Encounters | Establishes a clear, verifiable timeline of medical events. | Date, provider, encounter type, and Bates number or source page for every entry. |
| Diagnoses | Connects the incident directly to specific medical conditions. | All diagnoses linked to the incident, including ICD codes and the diagnosing provider. |
| Treatments & Medications | Details the full scope of medical care received. | Surgeries, therapies, prescriptions, and recommended future treatments. |
| Functional Impact | Quantifies the injury's effect on the client's daily life. | Limitations on work, daily activities, and long-term prognosis from provider notes. |
| Gaps & Inconsistencies | Proactively addresses potential weaknesses in the case. | Noted gaps in treatment, pre-existing conditions, or conflicting provider opinions. |
Having these components clearly defined and organized is the first step toward creating a summary that not only informs but also persuades.
Building a Defensible Chronological Framework
A persuasive medical summary isn't built on clever legal arguments; its foundation is a rock-solid chronological framework. This isn't about just listing events as they happened. It's about meticulously constructing a verifiable narrative that transforms a mountain of disorganized records into a clear, compelling story of cause and effect.
For the people who matter—insurance adjusters, opposing counsel, and mediators—a clean timeline is everything. When they can easily trace the path from the initial incident to the resulting diagnoses, treatments, and lasting impairments, your case instantly gains credibility. A jumbled summary forces them to play detective, which breeds skepticism and buries the facts you need them to see.
This visual captures the essence of the process: turning raw, chaotic records into a strategic advantage, all through the power of a well-structured summary.
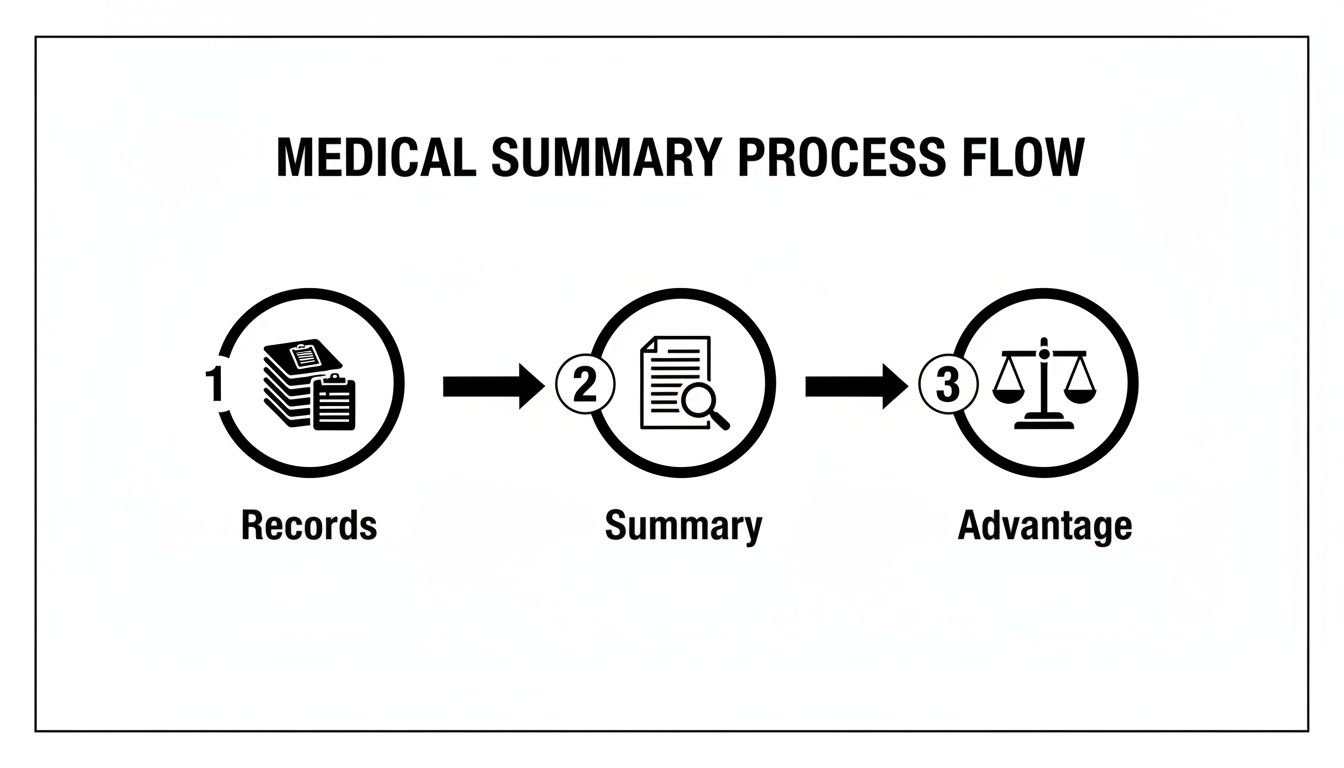
As the diagram shows, a clear summary format is the bridge that connects the raw data from medical files to a much stronger legal argument.
Mastering the Flow of Information
Creating this flow demands a strict, consistent approach for every single entry. Each patient interaction, from that first ER visit to a physical therapy appointment six months later, has to be documented with precision. This is where so many summaries miss the mark. They either get bogged down in useless detail or leave out the source identifiers that make the timeline trustworthy.
To nail this, every entry in your chronology needs these four elements:
- Exact Date of Service: The specific day is crucial, not just the month.
- Provider Name and Specialty: Clearly state who provided the care (e.g., "Dr. Evans, Neurologist").
- Type of Encounter: Was it an initial consult, an MRI, a surgical procedure, or a follow-up visit?
- Key Details: A brief note on the reason for the visit and its outcome.
Even more important is tying every single fact back to the source document with a Bates number or page identifier. This simple step is what makes your summary defensible. It empowers anyone reviewing the file to instantly verify a piece of information, shutting down any questions about accuracy. You're not just telling them what happened; you're showing them the proof.
Expert Tip: The goal of a chronological framework is to make the reader’s job effortless. If an adjuster can follow the client’s journey from injury to impairment without ever feeling lost or confused, you’ve already won a major battle.
Handling Multiple Providers and Complex Histories
Personal injury cases are rarely neat and tidy. Clients often bounce between ER doctors, orthopedic surgeons, primary care physicians, and multiple therapists. The real challenge is weaving these separate record sets into one coherent timeline that tells a single story.
The solution is a unified master chronology. Instead of summarizing each provider's records in a vacuum, integrate every encounter into one timeline, sorted strictly by date. This approach immediately clarifies the progression of care, reveals referral patterns, and makes any gaps in treatment glaringly obvious. For a deeper dive, our guide on crafting a detailed medical record chronology lays out more advanced strategies for this.
This isn't just a matter of preference; it's a proven industry standard that boosts efficiency. By organizing records this way—with consistent date ordering and source citations—you can cut a reviewer's search time by an estimated 30-50%.
Ultimately, building this defensible framework is about creating the undisputed source of truth for your case. It provides the logical backbone for every other argument you'll make about diagnoses, causation, and damages. Get this right, and you'll have a powerful tool that moves your case forward with confidence.
Structuring Key Sections for Maximum Impact
A solid timeline is the backbone of any medical summary, but the real story—the part that convinces an adjuster or opposing counsel—is told in how you structure the key sections. These aren't just data dumps; they're your chance to guide the reader, build a compelling argument, and translate complex medical jargon into a clear narrative of injury, treatment, and ongoing impact.
Get this part right, and an attorney can grasp the core facts of the case in minutes. Get it wrong, and your summary becomes a confusing recitation of facts instead of the powerful persuasive tool it needs to be. Each section has a job to do: the header provides quick context, the diagnosis establishes causation, the treatment log proves diligence, and the functional impact details what was lost.
This modular approach lets you control the flow of information, highlighting the most critical details right from the start.
To help you nail this, here's a look at how to build out each section, including what's essential and what common missteps can weaken your case.
| Medical Summary Section Blueprint | ||
|---|---|---|
| Section Name | Essential Information (Include) | Common Mistakes (Avoid) |
| Case Header | Client's full name, DOB, Date of Incident (DOI), case/claim number, and a brief case identifier (e.g., "MVA" or "Premises Liability"). | Omitting the DOI or claim number, forcing the reader to hunt for basic information. Using vague identifiers. |
| Encounter Chronology | A concise, reverse-chronological list of every medical encounter with dates, providers, and a one-sentence description. | Writing long, narrative paragraphs for each entry. Forgetting to link to the corresponding source page in the records. |
| Diagnoses | A clear list of all incident-related diagnoses, with ICD codes, the diagnosing physician's name, and the date of diagnosis. | Simply copying and pasting a list of medical terms. Failing to connect the diagnosis directly to the incident in the description. |
| Treatments | A logical summary of treatments (by type or provider), including dates, purpose, and outcomes. Shows compliance and diligence. | Creating a jumbled list of appointments. Not explaining why a treatment was necessary or what its results were. |
| Functional Impact | Direct quotes and physician notes on how injuries affect Daily Living Activities (ADLs), work, and hobbies. Quantify the loss. | Making vague statements like "client is in pain." Not including specific, documented limitations from the medical records. |
| Gaps & Inconsistencies | An objective section noting any gaps in treatment, pre-existing conditions, or conflicting patient statements. Addresses red flags proactively. | Ignoring problematic information or trying to hide it. This destroys credibility when the other side finds it. |
By following this blueprint, you create a document that's not only comprehensive but also strategically sound, making the reviewer's job easier and your arguments stronger.
Crafting the Case Header
Think of the case header as the summary's title page. It's the first thing anyone sees, so it needs to deliver instant context and all the essential identifying details at a glance. This is purely about facts, presented cleanly to avoid any administrative headaches down the line.
A well-constructed header must have:
- Client’s Full Name and Date of Birth: The non-negotiables for accurate identification.
- Date of Incident (DOI): This is the anchor for the entire medical narrative.
- Case or Claim Number: Crucial for cross-referencing with adjusters and other case files.
- Brief Case Identifier: A simple descriptor like "Motor Vehicle Accident" or "Slip and Fall at [Location]."
This is the file tab for your entire summary. If someone picks up this document, they should know who it’s about and what incident it relates to in under five seconds. Forcing them to dig for this basic info just starts the review process off with frustration.
Detailing the Initial Diagnosis and Prognosis
Right after the timeline, this is where you explicitly connect the incident to the medical fallout. Your job here is to list every diagnosis that stems directly from the event, translating dense medical terminology into plain English. The goal is to forge an undeniable link between the accident and the injuries.
For real punch, list each diagnosis on its own line. Make sure you include the specific ICD code, the name of the doctor who made the diagnosis, and the date it was recorded. This simple step adds a huge layer of clinical authority.
A common shortcut is to just copy a list of diagnoses from a patient chart. Don't do that. Instead, frame each one to tell the story. For example, instead of just "Cervicalgia," you should write: "Cervicalgia (neck pain) - Diagnosed by Dr. Evans on 01/15/2024, attributed to whiplash from the motor vehicle collision."
This section is also the perfect place to introduce the initial prognosis. If you can pull a direct quote from the physician's notes, do it. A line from an ER doctor like, "Patient will likely experience chronic pain and require long-term physical therapy," is incredibly powerful. It immediately sets the tone for the severity and expected duration of the client's recovery.
Summarizing Ongoing Treatments
Here, you're documenting the client's entire journey toward recovery. This section proves they were compliant with medical advice and shows the full scope of care they needed. It’s your best evidence for justifying medical bills and demonstrating just how hard your client worked to get better.
I find it's best to organize this section logically—either group treatments by provider or by type (e.g., Surgical Interventions, Physical Therapy, Pain Management). For every entry, you'll want to include:
- Treatment Type: Be specific. Not just "surgery," but "Arthroscopic knee surgery to repair medial meniscus tear."
- Provider Name and Facility: Who did the work and where it happened.
- Date Range of Treatment: From the start date to the end date (or simply "Ongoing").
- Purpose and Outcome: A quick note on why the treatment was done and how it affected the client's condition.
This systematic approach keeps the summary from turning into a messy list of appointments. It paints a clear picture of a necessary and methodical course of care, making it much tougher for an insurance company to claim the treatments were excessive or unrelated.
Finding and Fixing the Flaws in a Case
A great medical summary doesn't just list what's in the records; it digs deeper. It's about spotting the potential problems before the other side does. This is how you shift from simply reporting facts to creating a powerful strategic asset for your legal team. When you proactively identify issues like treatment gaps, pre-existing conditions, or even conflicting notes, you give your attorneys the chance to build a rock-solid case from day one.
Make no mistake, ignoring these red flags is a rookie move. Opposing counsel and insurance adjusters are paid to find these very weaknesses and use them to poke holes in your claim's value. By tackling them directly in the summary, you seize control of the story, show you have nothing to hide, and prove you've done your homework.
Pinpointing Gaps in Treatment
One of the first things an adjuster hunts for is a gap in treatment. If they see a client went weeks or months without seeing a doctor, they'll argue the injury must not have been that serious or was already healed. Your task is to find those gaps in the chronology and explain them right then and there.
Don't just let a huge chunk of time pass by silently in the timeline. You need to flag it with a simple, objective note.
- What a weak summary does: The chronology just jumps from an ER visit in January to a specialist appointment in April, leaving a gaping hole.
- What a strong summary does: Right after the January entry, it adds a clear note: "[Note: Records show a 12-week gap in care between 01/15/2024 and 04/10/2024. Client reported this delay was due to waiting for insurance pre-authorization for the specialist referral.]"
That one sentence completely changes the narrative. Suddenly, the gap isn't a sign of recovery; it's a frustrating but understandable administrative delay that jurors and adjusters can relate to.
Putting Pre-Existing Conditions in Context
Pre-existing conditions are another favorite target. The defense will jump at the chance to claim your client's pain is from an old issue, not the accident. A well-crafted summary anticipates this and draws a clear line in the sand.
The trick is to acknowledge the old condition head-on, then use the doctor's own words to show how this new incident made things demonstrably worse—an exacerbation or aggravation.
Don't try to hide a history of lower back pain. Instead, state it plainly. Then, pivot to the new evidence, using physician notes to prove the accident caused a significant, measurable spike in pain, a new loss of mobility, or the need for a much more aggressive treatment plan.
You could even create a specific section for this or just call it out in the chronology. For example, an entry could read: "Patient has a documented history of intermittent, manageable lower back pain (last treated 2022). Post-accident, notes from Dr. Smith on 03/05/2024 state 'acute exacerbation with new radicular symptoms,' which prompted an epidural steroid injection not previously required." Using direct quotes from the provider makes the distinction undeniable.
Handling Conflicting Information
Let's be honest, medical records are never perfect. You’ll find conflicting diagnoses between the ER doc and a specialist. You might even see the client's own account of the accident vary slightly from one visit to the next. Trying to sweep these inconsistencies under the rug is a terrible idea; it just makes you look dishonest when they inevitably come to light.
The best approach is transparency. A professional summary addresses these issues directly. You can add a small subsection called "Inconsistencies Noted" or simply place a brief, factual flag in the chronology where the conflict appears. You're not making excuses—you're just pointing it out. This gives the legal team a heads-up on exactly what they need to clarify with the client, so they can handle it gracefully in a deposition instead of being ambushed.
Using AI Tools to Enhance Your Summaries
Anyone who has manually drafted a medical summary knows the grind. It's a painstaking process of poring over hundreds, sometimes thousands, of pages, cross-referencing dates, and typing out every detail. Frankly, it's a workflow that's just begging for human error—a single misplaced decimal or an incorrect date can create real problems down the line.
This is where AI-powered platforms have completely changed the game. What used to be a multi-day slog for a paralegal can now be accomplished in minutes.
These tools aren't just about working faster; they bring a level of precision and verifiability that's hard to achieve by hand. By automatically pulling out key data points—encounter dates, diagnoses, treatments, providers—they build an accurate, structured timeline almost instantly. This frees up your team's time to focus on what actually matters: building a winning legal strategy.
This process is exactly how it works. AI takes that mountain of unstructured records and turns it into a clean, usable summary, closing the gap between raw data and actionable legal insight.
How AI Elevates the Standard Medical Summary Format
The real magic of these tools isn't just that they're faster, but that they produce a fundamentally better work product. The biggest advantage, in my experience, is source linkage. Instead of just listing a fact, the best AI platforms hyperlink every single entry directly to the source page in the original medical record.
This feature is a game-changer when it comes to defending your case. Imagine an adjuster questioning a specific treatment date. Instead of digging through a banker's box of records, you just click the link and instantly show them the exact page where that information appears. It shuts down challenges to your summary’s accuracy on the spot.
We're seeing this capability drive a higher standard across the industry. Firms using this kind of tech are reporting a 40–60% reduction in manual review time on cases with extensive records. It's quickly becoming the new baseline for efficiency and accuracy.
Choosing the Right AI Platform
Let's be clear: not all AI tools are created equal. As you look at different platforms for your firm, there are a few non-negotiable features you should be looking for.
A quality platform must offer:
- Automated Chronology Generation: The core function should be its ability to ingest thousands of pages and spit out a clean, date-sorted timeline of every medical encounter.
- Key Data Extraction: It needs to accurately pinpoint and extract critical information like diagnoses with ICD codes, medications, treating physicians, and facility names.
- Source Linking: This is critical. Every data point in the summary must be hyperlinked back to the original source document. Don't even consider a tool without it.
- HIPAA Compliance: The platform absolutely has to follow strict data security and privacy protocols. There's no room for error when handling protected health information.
Tools like Ares are built from the ground up for the specific needs of personal injury law. They do more than just extract data; they help draft initial summary narratives and can even give you a head start on demand letters. It creates a much smoother workflow from the initial record review all the way to settlement talks. If you're curious about this, check out our article on how AI can empower personal injury lawyers.
It’s crucial to remember that AI is a powerful assistant, not a replacement for legal expertise. The final summary always requires human oversight. An attorney’s critical eye is essential to interpret the data, craft the legal narrative, and ensure the summary aligns perfectly with the overall case strategy. AI handles the "what," but the legal team provides the "why."
Finalizing Your Summary for Compliance and Admissibility
Building a powerful medical summary is one thing, but making sure it’s legally sound is another. Before you send that document anywhere, there are a few final steps that are absolutely critical. This is where you move from just drafting to creating a defensible, compliant, and admissible piece of evidence. Getting this wrong can expose your client—and your firm—to unnecessary risk.
Think of this final quality check as your last line of defense. A rock-solid summary doesn't just tell a story; it serves as the factual backbone for other critical documents, especially when you're crafting a compelling settlement demand letter where every detail counts.
Adhering to HIPAA and Privacy Rules
Working with Protected Health Information (PHI) means walking a very fine line with the Health Insurance Portability and Accountability Act (HIPAA). A slip-up here isn't just a minor mistake; it can lead to massive penalties. We're talking civil fines that can climb past $2 million per violation.
Your first priority is protecting your client's privacy. Before that summary goes out the door, you have to comb through it and redact any information that isn't directly relevant to the personal injury claim.
You'd be surprised what can sneak in. Be on the lookout for sensitive details like:
- Social Security numbers (unless absolutely required for a specific filing).
- Notes about unrelated medical conditions that have no bearing on the case.
- Private information about family members who aren't involved.
Managing these records correctly is fundamental to our work. If you want to dive deeper into the specific protocols, our guide on HIPAA-compliant document management is a great resource.
The gold standard is simple: treat every piece of information as confidential unless its disclosure is absolutely essential to proving the case. When in doubt, redact it. This protects your client and shores up your firm's professional integrity.
Preparing the Summary for Evidentiary Submission
Once you've locked down compliance, the next step is to prepare the summary for review by courts, mediators, or opposing counsel. The goal is to make it easy for them to navigate and, more importantly, to verify. Every single statement in your summary must be directly traceable back to a source document.
A final review should be a non-negotiable part of your process, confirming a few key points to ensure the summary will withstand scrutiny.
Final Admissibility Checklist:
- Source Verification: Can you point to a specific Bates number or page in the medical records for every single entry, diagnosis, and treatment note?
- Objectivity Maintained: Have you stripped out all of your own commentary, opinions, or legal arguments? The summary must be a neutral presentation of medical facts, not your legal strategy.
- Clean Presentation: Is the document easy on the eyes? Think clear headings, a legible font, and plenty of white space. A messy, cluttered summary just looks unprofessional and is a pain to review.
By running through these checks, you elevate your medical summary from a simple report to a defensible work product ready for any legal battle.
Frequently Asked Questions About Medical Summaries
Even with the best templates, you'll inevitably run into questions when drafting a medical summary. The details really matter here—getting them right is what makes the document compelling and credible. Let's walk through some of the most common issues we see legal teams grapple with.
Chronological or Reverse-Chronological Order?
One of the first decisions you'll make is how to structure the timeline of encounters. While both chronological and reverse-chronological formats have their place, reverse-chronological is almost always the better choice for personal injury cases.
Why? Because it immediately shows the reviewer the client's current status. Starting with the most recent provider visit gives an instant, up-to-date picture of the client's condition and ongoing care needs, which is crucial for framing the damages conversation.
How Much Detail Is Too Much?
Another common sticking point is just how granular to get with each entry. Should you include every single minor complaint mentioned in the records? Absolutely not. The goal is to create a clear, powerful narrative, not a cluttered mess.
Each entry in the timeline should be a concise, one-sentence snapshot that gets right to the point—the purpose of the visit and its outcome.
A great entry isn't a long-winded paragraph. It's focused and efficient: "05/10/2024: Follow-up with Dr. Smith (Orthopedics) to review MRI results, confirming a partial rotator cuff tear; physical therapy frequency increased to 3x/week." This gives the reader everything they need to know without the fluff.
Where Does Billing Information Go?
Finally, there’s the question of billing. The medical summary is not the place for itemized bills or treatment costs. Its sole purpose is to tell the medical story: the injuries, the course of treatment, and the impact on the client's life.
Financial details belong in a separate damages summary or within the demand letter itself. Mixing them into the medical narrative only dilutes its impact and distracts from the core medical evidence. Keeping these two components separate makes both documents sharper and more effective.
Stop wasting hours on manual record review. Ares automates the creation of detailed medical chronologies and summary drafts, giving your team back valuable time to focus on strategy. See how it works at https://areslegal.ai.