Reviewing Medical Records for Attorneys A Modern Playbook
For any personal injury firm, mastering the medical record review process is the difference between a strong, defensible case and a logistical nightmare. It's not just about reading through pages of clinical notes. It’s about strategically dissecting a chaotic collection of patient files and transforming it into a clear narrative that proves causation and spells out damages.
The Modern Approach to Medical Record Review
Let's be honest: the old way of reviewing medical records is a major bottleneck. It chews up paralegal and attorney hours, drives up operational costs, and, worst of all, can leave gaps in your case. An effective review isn't just another task on the checklist; it's the bedrock of your entire legal strategy.
This guide outlines a modern, systematic approach that moves your team away from the mind-numbing, page-by-page slog. Instead, we’ll focus on a structured, tech-enabled workflow grounded in these core principles:
- Smart Organization: Building a logical, searchable file system from day one.
- Precise Data Extraction: Systematically pulling out critical details—diagnoses, treatments, providers, and dates.
- Compelling Chronology Building: Weaving that data into an undeniable, persuasive timeline.
- Strategic Analysis: Pinpointing the strengths, weaknesses, and direct evidence of causation buried in the records.
The Real Cost of Inefficient Review
Inefficiency isn't just a headache; it has a real, measurable impact on your cases and your firm's bottom line. With nearly 400,000 personal injury claims filed in the U.S. each year, medical records are the central pillar of proof.
Yet, the average personal injury firm sees a demand package delay of over 100 days on 42% of cases after a client's treatment ends. Why? Because teams get bogged down sifting through mountains of dense medical files. You can find more detail on this in these medical record review best practices for 2025.
This delay isn't just an inconvenience. It directly stalls your ability to negotiate settlements and move cases forward, turning a critical asset into a costly administrative burden. The goal is to make these records a tool that accelerates your workflow, not one that grinds it to a halt.
To fully appreciate the shift, it's helpful to compare the old way of doing things with a more current, technology-supported process.
| Aspect | Traditional Manual Review | Modernized AI-Powered Review |
|---|---|---|
| Initial Processing | Manually sorting and paginating hundreds of pages of paper or unorganized PDFs. | Automated document sorting, de-duplication, and categorization by provider or date. |
| Data Extraction | A paralegal or attorney reads every page, highlighting and manually typing key data into a separate summary. | AI tools automatically identify and extract key data points (diagnoses, treatments, providers, dates) in seconds. |
| Time Investment | Hours or days per case, depending on record volume. Highly repetitive and prone to human error. | Minutes to a few hours. Frees up legal staff to focus on analysis and strategy. |
| Accuracy | Susceptible to missed details, typos, and inconsistent data entry. | High degree of accuracy and consistency, with easy verification by linking directly to the source document. |
| Chronology Building | A manual, painstaking process of piecing together events and dates from notes and summaries. | Instantly generated, interactive timelines that can be filtered and searched. |
| Case Analysis | Relies solely on the reviewer’s memory and ability to connect disparate facts across a massive document set. | AI can flag missing records, identify treatment gaps, and highlight potential causation links for attorney review. |
This table makes it clear: embracing new tools isn't just about being "modern." It’s a strategic decision that directly translates to more efficient case management and better outcomes.
Embracing a Global and Digital Workflow
Our work is more interconnected than ever, which means we often receive medical records from different states, countries, and in multiple languages. A truly modern workflow has to be ready for this.
For cases involving multi-lingual records, for example, using specialized medical document translation services is no longer a luxury but a necessity for accuracy.
By adopting a structured workflow, you empower your team to spend less time on administrative drudgery and more time on high-value legal strategy. This shift doesn’t just get you to the settlement table faster—it strengthens your cases and positions your firm to handle a larger caseload with greater precision.
Organizing Case Files for Maximum Efficiency
Before you can ever hope to tell a compelling story for your client, you have to bring order to the chaos. Medical records rarely arrive in a neat, organized stack. They come in as a jumble of digital files, faxes, and paper, creating a mess that can easily lead to missed details and strategic blind spots.
The key is to establish a system so intuitive that anyone on your team—from a senior partner to a brand-new paralegal—can pull up a specific lab result or physician's note in seconds. This process starts the moment a record hits your desk. The temptation is to dive right in and start reading, but that's a mistake. Structure must come first.
Establishing a Bulletproof Audit Trail
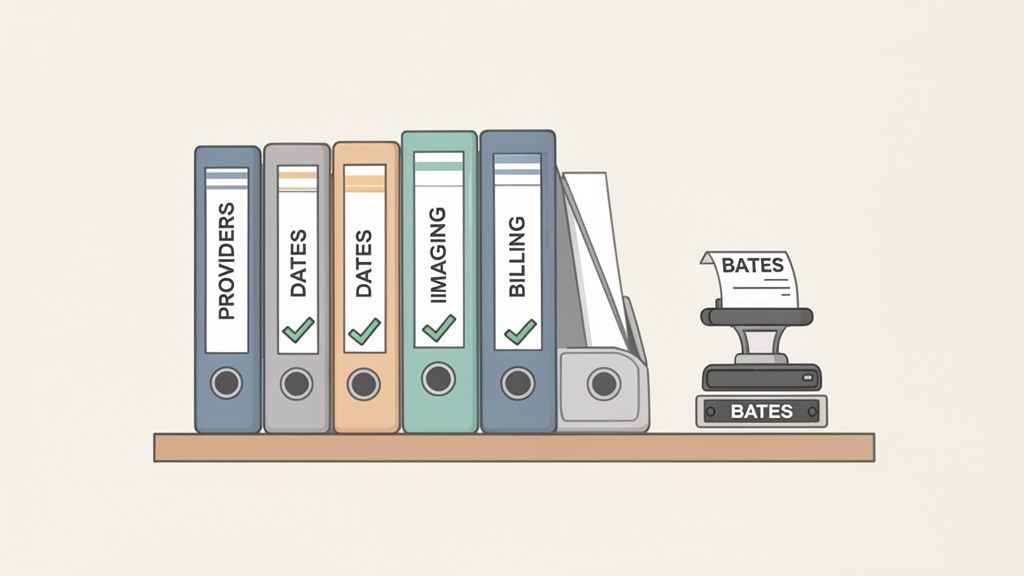
Your first move in any professional workflow for reviewing medical records for attorneys is to create a single, unified digital file. Every scrap of paper gets scanned, and all existing electronic documents are consolidated into one place.
From there, every single page gets a unique identifier through Bates stamping. This isn't optional; it's the foundation of a defensible case file. The sequential numbering system creates an ironclad audit trail, ensuring every page is accounted for and can be cited with precision in demand letters, depositions, and trial exhibits.
Think about the difference between telling an expert to "turn to page B-00178" versus "look for the third page of that ER report from sometime in June." The first is professional and undeniable. The second is an invitation for confusion and doubt.
A consistent Bates stamping system is a hallmark of a high-functioning personal injury firm. It shuts down ambiguity and provides a concrete reference point that holds up under scrutiny from adjusters and opposing counsel.
Once everything is stamped, it's time to hunt for duplicates. It's incredibly common for a single hospital visit to show up in records from the PCP, a specialist, and the hospital itself. A quick de-duplication pass can slash the page count, saving you a surprising amount of review time later on.
Creating a Logical Folder Structure
With a clean, stamped, and de-duplicated set of records, you can now build your organizational framework. A standardized folder structure is the backbone of an efficient practice, ensuring every case file is set up the exact same way.
A battle-tested approach involves sorting records into a clear hierarchy. We get into the weeds on this topic in our detailed guide on how to organize medical records for legal cases.
Here’s a simple structure that works for the vast majority of personal injury files:
- Primary Folder: [Client Last Name, First Name] - [Case Number]
- Subfolder 1: By Provider
- St. Mary's Hospital
- Johnson Orthopedics
- Metro Physical Therapy
- Subfolder 2: By Document Type
- Physician's Notes
- Imaging Reports (X-rays, MRIs)
- Billing Statements & Invoices
- Prescription Records
- Subfolder 3: Chronological
- A single, merged PDF of all records, sorted by date of service.
- Subfolder 1: By Provider
This multi-faceted system gives you incredible flexibility. Need to see everything from a specific doctor? Jump into the "By Provider" folder. Trying to calculate damages? The "By Document Type" folder has all your bills in one place. And the chronological file is your secret weapon for building the case timeline later.
Handling Problematic Records
Let's be realistic—not all records arrive in pristine condition. You're going to get illegible handwritten notes, blurry faxes, and files with obviously missing pages. Don't just ignore them.
Set up a dedicated subfolder named "For Review" or "Problem Docs." When you find a problem record, drop a copy in there and create a running memo that lists each one. Your memo should track the document's Bates number, provider, date, and the specific issue (e.g., "Handwriting on SOAP note unreadable," or "Report says page 3 of 5, but page 4 is missing").
This turns a potential oversight into a clear action list. Now you have a documented basis for follow-up requests to the provider, ensuring these critical issues don't get lost in the shuffle as the case moves forward. This is the kind of meticulous groundwork that transforms a mountain of paper into a strategic asset.
Finding the Story in the Records: How to Extract Case-Winning Data
Once you’ve got the records organized, it’s time to roll up your sleeves. This is where the real case-building happens. You’re about to transform a mountain of paper into a powerful, persuasive narrative that connects the dots from the incident to your client’s current condition.
This isn’t just about making lists. It’s a meticulous hunt for the specific data points that will form the backbone of your demand letter and, if needed, your trial presentation. A haphazard approach here will result in a weak, disjointed story. What you need is a systematic way to pull the same critical details from every single record, no matter who wrote it or what format it’s in.
The Data Points That Matter Most
Think of yourself as a detective. You're searching for every clue that links the client's medical journey back to the negligence that caused their injury. To do this right, you need a mental checklist of what to look for every single time.
Here’s what I always look for:
- Key Dates: This is the skeleton of your timeline. Nail down the date of injury, the first treatment, every follow-up, every surgery, and every physical therapy session.
- Providers and Facilities: Who treated the client and where? List every single doctor, specialist, therapist, and hospital. This creates a map of the client's entire care network.
- The Specific Diagnoses (with ICD Codes): "Back pain" isn't good enough. You need the precise diagnosis and its ICD-10 code, like S32.0 for a lumbar vertebra fracture. These codes are the universal language of medicine and are non-negotiable for proving the exact injuries.
- Treatments and Medications: Every procedure, therapy, and prescription needs to be documented. Make sure to note dosages and frequency—this detail paints a vivid picture of the severity of their condition.
- Pain and Suffering (in their own words): This is gold. Look for the subjective notes from the providers. Phrases like "patient reports 8/10 pain," "difficulty sleeping due to pain," or "unable to perform daily household chores" are powerful quotes that give a voice to the client's suffering and build your case for non-economic damages.
When you consistently pull this information, you create a clean, structured dataset. From there, building out a compelling medical chronology becomes exponentially easier.
Putting It All Together: A Real-World Example
Let's walk through a common scenario: a client who was rear-ended and now has neck pain. The initial records have landed on your desk—the ER report, notes from an orthopedic follow-up, and the first few physical therapy session notes.
From the ER Report:
First, you grab the date of the incident and the client's chief complaints: "neck pain" and "headache." The diagnosis is a "Cervical sprain/strain" (ICD-10: S13.4). You also note they were given a muscle relaxant and told to see an orthopedist.
From the Orthopedist's Notes:
Two weeks later, the client sees the specialist. You pull the specialist’s name and the date of the visit. The notes not only confirm the cervical strain but add a new diagnosis: "Post-traumatic headache" (ICD-10: G44.309). Then you find the money quote: a note from the doctor stating, "Patient's symptoms are directly consistent with the mechanism of injury from the motor vehicle accident described." Boom. That’s a direct link to causation.
From the Physical Therapy Records:
Here, you extract the therapy start date and the prescribed frequency, like "3 times a week for 6 weeks." You hunt for notes on their functional struggles, like "limited cervical range of motion" or "patient reports pain when lifting anything over 10 pounds." This is the data that quantifies how the injury is actively disrupting their life.
You see what's happening? By pulling these specific data points from different records, you're not just creating a summary. You are actively weaving a story that starts at the crash and flows through every step of their treatment, with each new piece of data reinforcing the last.
Spotting the Red Flags Before the Defense Does
A truly expert review isn't just about finding the good stuff. It's about finding the potential problems in your case before the defense attorney does. Trust me, they're looking for these holes, so you need to find them first.
Keep an eye out for these common red flags:
- Pre-existing Conditions: Did the client already have a history of back issues? You need to know. Make a note of any mention of prior injuries or similar symptoms. This doesn't sink your case, but you have to be ready to clearly separate the old injury from the new, aggravated one.
- Gaps in Treatment: A big, unexplained gap between appointments is a gift to the defense. They'll argue the injury wasn't that serious or that something else must have happened in that time. If there's a three-month delay between the ER visit and seeing a specialist, you need to find out why and have an answer ready.
- Inconsistent Pain Complaints: If the client told the ER doc their pain was a 4/10 but later told a specialist it was a 9/10, you can bet the defense will point it out. There's often a good reason—pain can flare up—but you must anticipate this attack.
Finding these issues early on is a strategic advantage. It lets you build a response right into your case narrative from the beginning. You can address the gap in treatment head-on in your demand letter, armed with a good explanation, instead of getting blindsided in a deposition. This is how you turn potential liabilities into just another part of the story.
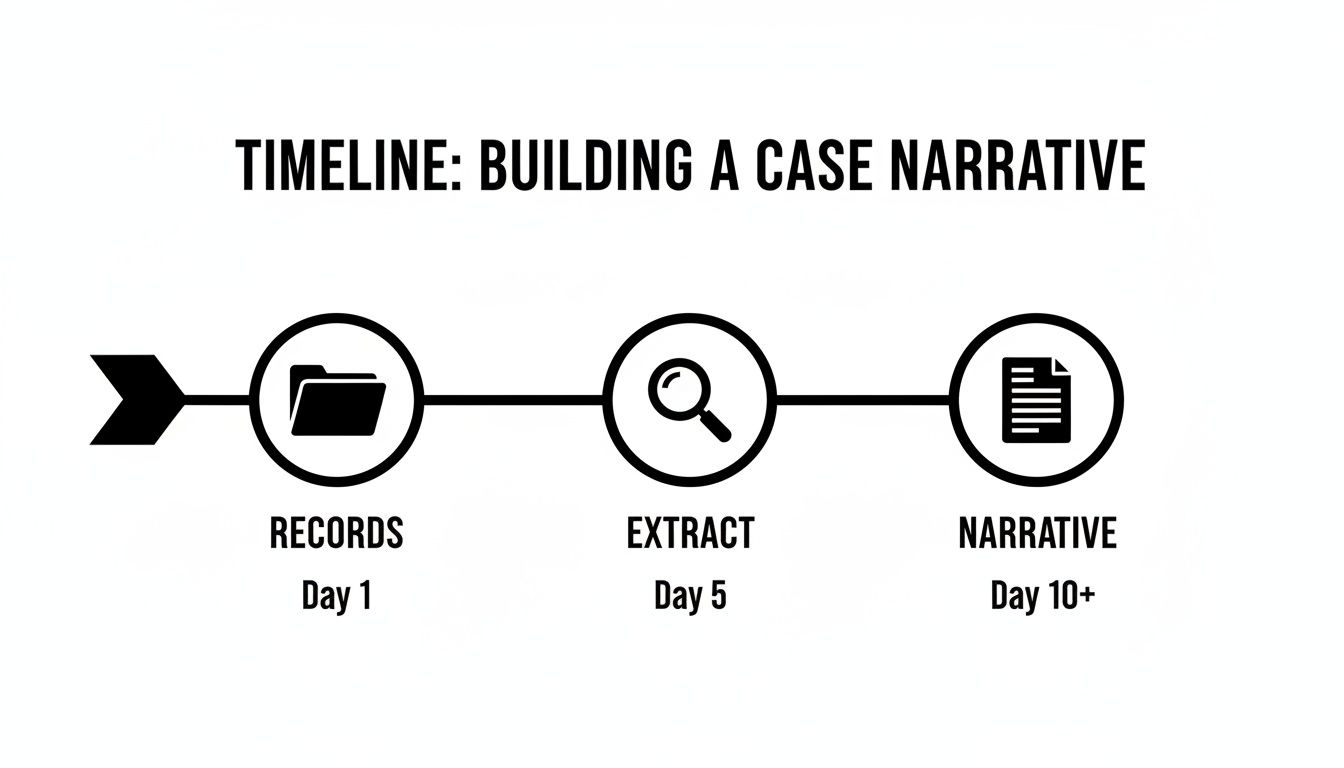
Constructing a Compelling Medical Chronology
Once you’ve sorted through the stacks of records and pulled out the essential data, you’re ready for the most critical part of the process: building the medical chronology. This isn't just about listing dates and appointments in order. A truly powerful chronology weaves everything—symptoms, treatments, doctor’s notes, and patient outcomes—into a cohesive story.
This is how you transform a pile of clinical paperwork into a clear, persuasive narrative that draws a direct line from the incident to your client's entire medical journey. For an adjuster or juror, a well-crafted chronology makes a complicated medical history easy to grasp, powerfully showing the full scope of your client's pain, suffering, and path to recovery.
This visual captures the essence of that workflow, moving from chaos to clarity.
As you can see, organizing the files and pulling out key data are the foundational steps. Without them, you can't build a narrative that will stand up to scrutiny.
Timeline vs. Chronology: Know the Difference
It’s easy to use these terms interchangeably, but in personal injury law, they serve two very different purposes. Getting this distinction right is key to building a stronger case.
- A Timeline: Think of this as the high-level summary. It’s a simple, linear list of major events: the date of the accident, the first ER visit, the orthopedic follow-up, the start of physical therapy. It’s great for getting your bearings but lacks the persuasive detail you really need.
- A Medical Chronology: This is where the story comes to life. It’s a much more detailed, narrative-driven document. A chronology takes all those timeline events and enriches them with the crucial context—symptoms reported at each visit, specific diagnoses, prescribed treatments, and even direct quotes from provider notes that touch on causation or prognosis.
A timeline gives you the skeleton. The chronology adds the muscle and sinew, creating a living, breathing account of your client's experience. It's no surprise that a recent study found 48% of legal teams now favor detailed chronologies for the deeper, event-driven insights they provide.
Building Your Chronology: A Practical Framework
The best way to build your chronology is to start with a simple table or spreadsheet. This forces you to capture consistent information for every single medical encounter, which is absolutely essential for creating a coherent narrative.
Here’s a practical template I’ve used countless times:
| Date of Service | Provider / Facility | Summary of Visit / Treatment | Key Findings & Diagnoses | Causation Notes / Red Flags |
|---|---|---|---|---|
| 01/15/2024 | St. Mark's ER | Pt presented post-MVA c/o neck pain, headache. X-ray performed. | Cervical strain (S13.4). Rx muscle relaxants. | Notes state "patient was restrained driver in rear-end collision." |
| 01/29/2024 | Dr. Evans, Ortho | Follow-up for persistent neck pain. Physical exam noted limited ROM. | Confirmed cervical strain; added Post-Traumatic Headache (G44.309). | Dr. Evans noted: "Symptoms are consistent with mechanism of injury." |
| 02/05/2024 | Premier PT | Initial physical therapy eval. Started on 3x/week plan for 6 weeks. | Pt reports 7/10 pain. Difficulty lifting >10 lbs. | PT goals focus on returning to pre-accident functional status. |
This structured approach does more than just organize dates. It forces you to actively hunt for the connections, the expert opinions, and the real-world impacts of the injury at every stage. This granular work is the foundation of a rock-solid demand package. For a deeper dive, check out our complete guide on creating a medical record chronology.
A powerful medical chronology is the central truth of your case. It’s the one document that allows anyone—an adjuster, a mediator, or a jury—to walk through your client’s journey and arrive at the undeniable conclusion that the incident caused the documented harm.
Visualizing the Narrative for Maximum Impact
Once your detailed chronology is built, your last thought should be presentation. For demand letters, that table format is often all you need. But when you’re heading to mediation or preparing trial exhibits, a visual timeline can be incredibly persuasive.
You can use tools like PowerPoint, Canva, or specialized legal graphics software to turn your detailed chronology into a clear, easy-to-follow graphic. A visual can instantly highlight key events like surgeries, show the full duration of treatment, and make any gaps or periods of intense medical care immediately obvious.
By turning your meticulous data into a compelling visual story, you make complex medical facts accessible and memorable. You ensure your client's experience isn't just read about, but truly understood.
Putting AI to Work: Streamlining Your Medical Record Review
Let's be honest: the old-school, page-by-page slog through medical records isn't just tedious—it's fast becoming a competitive disadvantage. What used to be a futuristic concept is now a practical tool that directly solves the biggest headaches in personal injury work: the enormous time sink, the mounting costs, and the ever-present risk of human error.
Modern AI platforms are built for this. They can take thousands of pages of jumbled records and, in just a few minutes, pull out the exact data points you need to build your case. This isn't about replacing legal expertise. It’s about augmenting it. The goal is to hand off the most mind-numbing, repetitive tasks so your team can focus on what really matters: strategy, client relationships, and building a case that wins.
Breaking Through the Manual Review Bottleneck
The raw numbers behind manual review are staggering. Firms often see demand packages delayed by over 100 days in 42% of cases, simply because of the sheer labor involved in sorting through post-treatment records. Think about it: a single 1,000-page file can easily chew up 15+ hours of a paralegal's time, costing the firm over $500 in billable hours.
This is exactly why 56% of personal injury lawyers say medical record summarization is their number one priority for AI.
AI-powered platforms completely change this math. They’re trained on millions of medical documents, so they know exactly what to look for and how to categorize it. You simply upload the files, and the system gets to work.
What you’re seeing here is the end of manual sorting. The AI handles the intake, organization, and initial analysis, freeing your team to do the work that requires their critical thinking skills.
How AI Uncovers Case-Winning Intelligence
Think of these tools as a hyper-efficient paralegal who never gets tired or needs a coffee break. The AI reads every single page and extracts the crucial details with impressive accuracy.
Here’s what these platforms do best:
- Automated Data Extraction: It instantly identifies and pulls key data like diagnoses (complete with ICD codes), specific treatments, medications, provider names, and all relevant dates.
- Chronology Generation: Instead of you or a paralegal spending hours building a spreadsheet, the platform generates a clean, chronological timeline of every medical event in minutes.
- Symptom and Pain Tracking: The system can pinpoint every mention of pain, symptoms, and the client's own words describing their struggles—gold for proving non-economic damages.
- Gap and Inconsistency Spotting: AI is great at flagging things a human reviewer might miss after hours of reading, like long gaps in treatment or conflicting notes from different providers.
A real-world example: Imagine your client missed a month of physical therapy. An AI tool would immediately flag that gap. You can then proactively ask the client for an explanation—maybe they had the flu or a family emergency. This lets you address a potential weakness head-on, long before the defense attorney brings it up in a deposition.
This shifts your entire process from reactive to proactive. For a closer look at how this plays out in a firm, you can read about how AI is transforming case management for personal injury lawyers.
The Real-World Benefits for Your Firm
Bringing AI into your workflow does more than just save time; it creates a cascade of positive effects across your whole practice. It gives you a better handle on complex information and helps you build much stronger arguments. To see more practical applications, check out our guide on the best ways to use AI for personal injury lawyers.
Firms that embrace this technology consistently see a few key improvements:
- Handle a Higher Caseload: By cutting 10+ hours of manual work from each case, your team can manage more files without getting burned out or letting quality slip.
- Settle Cases Faster: When summaries and timelines are ready in minutes, demand letters go out the door sooner. This simple change can dramatically shorten the entire settlement timeline.
- Improve Accuracy: AI significantly reduces the small human errors—a typo in a date, a missed detail in a doctor’s note—that can poke holes in your case. It provides a reliable, consistent foundation for your arguments.
- Ensure HIPAA-Compliant Security: Reputable AI platforms are built with enterprise-grade security and are fully HIPAA compliant, so you can manage sensitive Protected Health Information (PHI) without worry.
By automating the drudgery of medical record analysis, you empower your team to focus their talent where it counts. You can turn what was once a dreaded administrative chore into a genuine strategic advantage that helps you claim bigger and settle faster.
Common Questions About Reviewing Medical Records
Even the most seasoned legal teams run into questions when digging into complex medical files. The process is filled with nuances, from deciphering messy handwriting to navigating strict privacy laws. Here are some of the most pressing questions we hear from personal injury firms every day, along with practical advice you can put to work immediately.
What Is the Most Common Mistake to Avoid?
By far, the most frequent and costly mistake is failing to build a comprehensive medical chronology. Too many firms just summarize individual provider records in isolation. This creates a scattered, disjointed picture of the client's journey.
A siloed approach completely misses the story. A proper chronology connects the dots between different doctors, specialists, and therapists, showing a clear, continuous line of causation from the incident to ongoing treatment. Without it, you'll struggle to prove the full scope of damages, fight back against claims of pre-existing conditions, or explain away any gaps in care.
Another huge error is glossing over the billing records. These documents are gold for proving economic damages. Plus, they sometimes reveal treatments or diagnoses that aren't clearly detailed in the clinical notes, giving you another layer of evidence to work with.
How Should We Handle Missing or Incomplete Records?
Missing records can feel like a major roadblock, but a methodical approach usually solves the problem. It all starts with meticulous tracking. You need a system to document every single record request you send and to persistently follow up with providers who are dragging their feet.
If records are still missing after you’ve done your due diligence, it's time to figure out what that means for the case.
- What specific information is gone? Is it a key diagnostic report? A specialist's follow-up notes?
- How critical is that missing piece to proving causation or damages?
For truly vital documents, you might need to escalate. That could mean sending a certified letter directly to the provider's records custodian or, in more stubborn cases, issuing a subpoena. It's also a smart move to address the gap head-on in your demand letter. By stating which records are still outstanding and why you requested them, you show you've done your homework and prevent the defense from springing it on you as a surprise.
Proactively addressing missing records shows transparency and control over your case narrative. It signals to the opposing side that you have a thorough command of the facts—even the ones you don't have in hand yet.
How Does HIPAA Affect Our Review Process?
The Health Insurance Portability and Accountability Act (HIPAA) is the bedrock of patient privacy. For attorneys, compliance isn't just a good idea—it's a core professional duty that governs every single thing you do with medical documents.
First and foremost, you must get a valid, signed authorization from your client. This document has to specifically permit the release of their Protected Health Information (PHI) to your firm for their legal case. It needs to be crystal clear about which records can be obtained from which providers.
Once those records are in your hands, your firm has a legal and ethical obligation to protect that PHI. That means implementing serious security measures for both your digital and physical files.
Key Security Measures:
- Encrypted Storage: All digital records should live in an encrypted environment to block unauthorized access.
- Access Controls: Only team members who absolutely need to see sensitive case files should have access.
- Secure Communication: Never send PHI over unsecured email or messaging apps.
Using a HIPAA-compliant platform for case management isn't a luxury anymore; it’s a necessity. These systems are built with the safeguards required to meet federal privacy and security standards. They protect your client, your case, and your firm from the kind of data breaches that can be professionally and financially devastating.
Ready to transform your medical record review from a bottleneck into a strategic advantage? Ares provides an AI-powered platform built for personal injury firms to save time, claim bigger, and settle faster. Eliminate 10+ hours of manual work per case and build stronger, data-driven demand letters in minutes.