What is maximum medical improvement: A Practical Guide to MMI in Personal Injury
In any personal injury case, there’s a moment when the entire focus shifts. That moment is the declaration of Maximum Medical Improvement, or MMI. It’s a pivotal point where a doctor concludes that a client's medical condition has stabilized and isn't expected to get substantially better, even with more treatment.
This isn’t just medical jargon; it's the starting gun for accurately calculating the true, long-term value of a personal injury claim.
The True Meaning of Maximum Medical Improvement
Imagine recovering from a serious injury is like rebuilding a house after a tornado. The first phase is all about intense, active work—the emergency response, framing the new structure, and putting on the roof. This is the "active treatment" phase, where every effort is focused on healing and getting function back.
Maximum Medical Improvement is the point when the general contractor hands you the keys. The major construction is done. The foundation is solid, the walls are secure, and the house is as repaired as it's going to be.
This doesn't mean the house is perfect. There might still be painting to do, landscaping to finish, or even a need to install a ramp for accessibility. In the same way, reaching MMI doesn't mean a patient is 100% healed or free from pain. It simply means their primary condition has hit a plateau.
From Healing to Valuation
The declaration of MMI fundamentally changes the direction of a personal injury case. Before MMI, the focus is squarely on the present: managing active medical care and making sure the immediate bills get paid. After MMI, the focus shifts to the future.
Maximum medical improvement (MMI) is not a medical abstraction; it is a statistically measurable milestone that drives case valuation... Once MMI is reached, the case typically shifts from a “healing” phase to a “valuation” phase, where permanent impairment, future care, and work capacity are quantified for settlement or award. You can find more details on why MMI is a pivotal point in personal injury and workers' compensation claims on the Brandon J. Broderick website.
Trying to settle a case before the client reaches MMI is a huge gamble. It’s like selling that storm-damaged house before you have the final invoices from the contractors—you're almost guaranteed to undervalue it and leave a significant amount of money on the table.
This table shows just how dramatically the case changes once MMI is established.
The MMI Shift From Active Treatment to Case Valuation
| Case Aspect | Before Reaching MMI | After Reaching MMI |
|---|---|---|
| Primary Goal | Facilitating and documenting active medical treatment. | Quantifying long-term damages for a settlement demand. |
| Medical Bills | Focus is on current and accumulating expenses. | Focus shifts to projecting the costs of future care. |
| Damages | Unknown and constantly changing as treatment progresses. | Can be calculated with a high degree of certainty. |
| Case Focus | Proving liability and covering ongoing medical needs. | Proving the full extent of permanent losses. |
Once a physician has confirmed MMI, your legal team can finally build a complete and defensible damages model. This is where you can confidently calculate:
- Permanent Impairment: With the condition stabilized, a doctor can assign a permanent impairment rating, which is a specific percentage quantifying the client's loss of function.
- Future Medical Costs: The need for future care—like pain management, physical therapy, or assistive devices—can be projected with medical certainty.
- Lost Earning Capacity: The permanent impact on your client's ability to do their job and earn a living can be properly calculated and argued.
How Doctors and Experts Determine MMI
Figuring out when someone has reached Maximum Medical Improvement isn't as simple as flipping a switch. It's a careful clinical judgment, pieced together from a mountain of evidence. Think of the doctor as a detective meticulously reviewing the entire arc of a patient's recovery. They aren’t looking for a single, dramatic event, but for a clear and consistent pattern that says, "the healing phase is over."
This process isn't arbitrary. It’s a systematic review of the whole treatment history to find that specific point where the patient’s condition has essentially leveled out. In other words, it's the moment when more curative treatments are unlikely to bring about any significant improvement.
This shift from active recovery to a stable, long-term condition is a pivotal moment in any personal injury case.
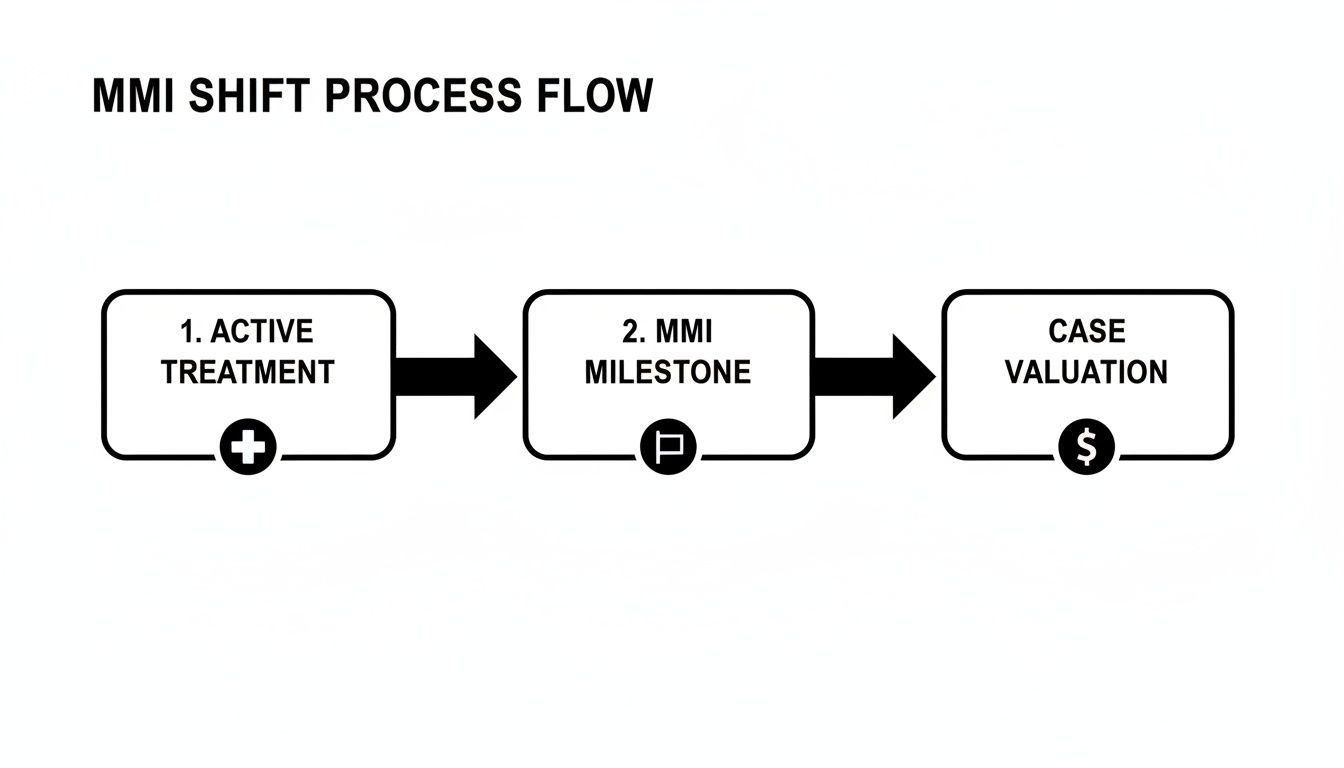
As you can see, the MMI declaration acts as the crucial bridge, moving a case from the active treatment phase into the final valuation and settlement stage.
The Role of the Treating Physician
The client’s own treating physician is almost always the primary source for an MMI opinion. This is the medical professional who has been in the trenches, witnessing the recovery journey firsthand. Their notes and reports form the bedrock of the MMI determination.
A doctor forms this judgment by tracking several key factors over time. They look for signs that the injury has truly stabilized—things like pain levels and functional limitations that are no longer improving or worsening. They also assess the effectiveness of treatments like physical therapy, noting when a patient hits a wall and stops making progress despite their best efforts. These observations, carefully documented over weeks or months, build the case for MMI.
"Maximum medical improvement occurs when no further marked change in a condition can be expected, regardless of whether additional medical treatment is provided. It signifies that the claims examiner determined, based on the statement by the rating or treating physician, that additional medical services wouldn’t lead to meaningful improvement."
This is a critical distinction. It’s the line that separates active, "curative" care from the long-term, "palliative" care that simply helps manage symptoms.
Independent Medical Examinations as a Counterpoint
While the treating physician's opinion is foundational, it's rarely the only voice in the room. The defense will often call for an Independent Medical Examination (IME). This is a one-time evaluation by a doctor hired by the insurance company to offer a second opinion on your client's condition.
Let's be clear: the goal of a defense IME is often strategic. The insurer might argue that the claimant reached MMI months ago and that any ongoing treatment is no longer reasonable or necessary. The IME doctor reviews the records, performs an exam, and issues a report with their own opinion on MMI status. This frequently creates a "battle of the experts," which is a common flashpoint in personal injury litigation.
Evidence Used in the MMI Determination
Whether it's the treating doctor or an IME, physicians rely on specific evidence buried within the medical records to back up their conclusions. Knowing what to look for is key to understanding—and sometimes challenging—an MMI finding.
Here are the key evidentiary components they scrutinize:
- Clinical Notes: These day-to-day entries are gold. They document symptom consistency, pain scores, and functional abilities. A pattern of no significant change over several visits is a powerful indicator of MMI.
- Therapy Reports: Notes from physical or occupational therapists are invaluable. They track objective data like range of motion and strength measurements, giving you concrete numbers on whether a patient is still progressing.
- Diagnostic Imaging: Comparing an MRI from the beginning of treatment to one from six months later can show if a physical injury has structurally healed or stabilized.
- Functional Capacity Evaluations (FCEs): These are comprehensive, standardized tests that assess a person's real-world ability to perform tasks, offering an objective measure of their permanent physical limits.
Sifting through hundreds of pages of these records is a huge task. Creating an efficient medical record summary is the best way to pull out the most relevant entries and build a clear timeline. This organized view makes it far easier to pinpoint the exact moment a patient's progress stalled and build a strong, evidence-based argument for when MMI was truly reached.
When you're navigating a personal injury or workers' compensation claim, you'll hear a lot of specific terms thrown around. Precision matters. One of the most important concepts is Maximum Medical Improvement (MMI), but you might also hear a similar-sounding phrase: Permanent and Stationary (P&S).
Are they the same? For the most part, yes. But the subtle differences can have a big impact on a case, especially depending on where you practice.
Think of it this way: MMI is the clinical judgment that a patient's condition has stabilized. P&S is often the legal trigger that follows. It's like a chef saying a dish is cooked (MMI), versus the waiter officially placing it on the table to be served (P&S). Both mean the cooking is done, but one moves the process to the next formal stage.
In many states, MMI is the common term used across all personal injury cases. However, some workers' compensation systems, like California's, rely on the official "Permanent and Stationary" designation to formally push a claim toward closure and the calculation of permanent disability benefits. The key is knowing which term carries weight in your specific jurisdiction and case type.
How This Connects to Impairment Ratings
Here’s the most important takeaway: a client reaching either MMI or P&S is the necessary first step before a permanent impairment rating can be assigned. You simply can't have one without the other.
An impairment rating is the number—a percentage—that a doctor assigns to quantify the permanent loss of function a client has suffered. It’s a foundational piece of evidence for calculating what a case is truly worth in the long run. A doctor can't possibly assign a permanent rating if the client's condition is still changing. That would be pure guesswork.
Reaching MMI or P&S is the green light. It signals that the medical picture has come into focus. Before that point, the client's condition is still a moving target, making any final assessment of damages premature and speculative.
This isn't just a medical timeline; it's a critical part of your case's narrative. It creates a logical, defensible story: the injury happened, the client treated until they hit a stable plateau (MMI/P&S), and only then could the full, lasting impact be measured.
A Real-World Example
Let's walk through a common scenario to see how this plays out.
- The Injury: Your client tears their rotator cuff in a collision and needs surgery to repair it.
- The Treatment Phase: For the next nine months, the client is diligent with their post-op physical therapy. They make great strides at first, regaining strength and movement.
- The Plateau: Then, the progress stops. The physical therapy notes for the last six weeks show the client's range of motion hasn't improved. Their pain, while better than before surgery, is now at a consistent, chronic level. They’ve hit a wall.
- The MMI Declaration: Seeing this sustained plateau, the orthopedic surgeon writes a report stating the client has reached Maximum Medical Improvement.
- The Impairment Rating: Now that MMI is officially on the record, the surgeon can proceed. They conduct a final functional exam and, referencing the official medical guidelines, assigns a 15% permanent impairment rating to the shoulder.
This sequence is everything. That 15% rating, which will be a central pillar of your settlement demand, only has credibility because the doctor first established that the client's recovery had concluded. Getting this order right ensures your valuation of the claim is built on solid ground.
The Role of MMI in Settlement Negotiations

When a doctor declares Maximum Medical Improvement, it's more than just a medical opinion. It’s the critical moment when theory translates into dollars and cents, forming the bedrock for a personal injury claim’s true financial value. Without it, you’re just navigating settlement talks in the dark.
Trying to settle a case before your client reaches MMI is like trying to price a house while it’s still being built. You can see the foundation and maybe some framing, but you have no real idea about the final layout, the quality of the finishes, or its ultimate market value. You're just guessing, and any offer you accept will almost certainly be a lowball.
Turning Medical Stability into Financial Clarity
Once MMI is established, the fog of uncertainty finally lifts. Your legal team can pivot from managing a client’s ongoing treatment to confidently calculating the full scope of their damages. This is the point where you can translate abstract suffering into concrete numbers, building a powerful and defensible demand letter.
The MMI date provides the definitive end to the medical narrative, giving you the evidence needed to argue for specific damages with total precision. This includes:
- Future Medical Needs: You can now clearly project the long-term costs of palliative care, whether it’s pain management injections, maintenance physical therapy, or prescriptions needed to manage chronic symptoms for years to come.
- Permanent Disability: A stable condition allows a physician to assign a permanent impairment rating, a figure that directly correlates to the value of a client's lost function.
- Lost Earning Potential: With a clear picture of the client’s permanent limitations, you can accurately model how their injuries will impact their ability to work and earn a living for the rest of their life.
This shift allows you to negotiate from a position of strength, armed with a complete and unassailable picture of your client's losses. It ensures the final settlement reflects the entirety of their journey—not just the initial phase of recovery. For a deeper dive into the numbers, check out our guide on the maximum medical improvement payout.
The Timing of MMI and Its Link to Claim Value
How long it takes a client to reach MMI isn't just a procedural detail; it’s a powerful indicator of the injury's severity and, by extension, the claim's value. It’s simple, really: more serious injuries require longer and more complicated treatment before a doctor can say the condition has stabilized.
Hard data from the workers' compensation world backs this up. A major study by the National Council on Compensation Insurance (NCCI) across more than 25 states found that for permanent partial disability claims, the average time to reach MMI was 363 days. Think about that—almost a full year from the date of injury. This research shows a clear statistical link between longer recovery periods, higher levels of permanent impairment, and, ultimately, higher claim values. You can read more about the NCCI research on impairment ratings for yourself.
A premature MMI declaration is a classic defense tactic. It's an attempt to put a cap on medical expenses and downplay the value of permanent damages. A well-documented, longer treatment history leading to a later MMI date inherently builds a stronger case for a higher settlement.
Understanding this dynamic is crucial. It reframes the MMI date from a simple medical milestone into a strategic asset. It proves that the client's condition was serious, required extensive care, and left lasting consequences that demand full compensation. It’s the objective proof that justifies a substantial settlement.
Streamlining MMI and Case Valuation with AI
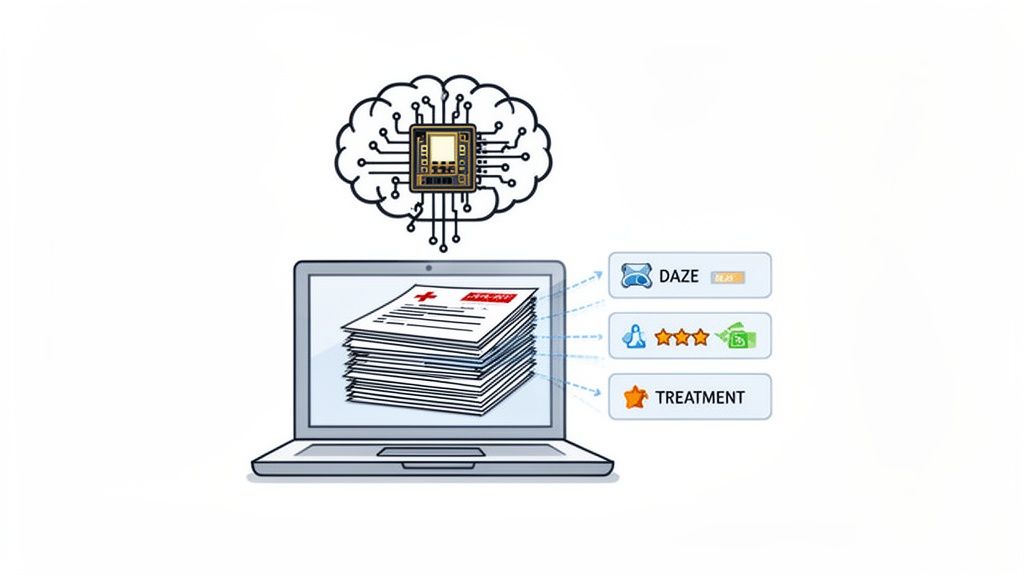
Knowing what is maximum medical improvement is one thing. Finding the doctor's official declaration of it buried in a mountain of medical records is a completely different challenge. For most personal injury firms, this is a tedious job for a paralegal or attorney, forcing them to manually sift through hundreds, often thousands, of pages of clinical notes.
This manual grind isn't just slow—it’s a high-stakes game where one missed detail can derail an entire case valuation. Overlooking the MMI date, a permanent impairment rating, or a subtle note about future care can mean leaving serious money on the table.
The Old Way: A Manual Bottleneck
The traditional way of finding an MMI declaration is a masterclass in inefficiency. It involves a painstaking, page-by-page review of records from different providers, all with their own formatting quirks and dense medical jargon. It’s a process riddled with risks that hit a firm’s bottom line directly.
A manual workflow usually looks like this:
- Time-Intensive Labor: It’s not uncommon for paralegals to spend over 10 hours per case just reading and summarizing medical files to pinpoint the key MMI-related data.
- High Risk of Human Error: In a document stack thousands of pages deep, it is shockingly easy to miss the one sentence where a doctor declares MMI, especially if it's tucked away in a routine progress note.
- Inconsistent Data Extraction: Different team members might interpret or flag information differently, which leads to inconsistent case summaries and wobbly demand letters.
- Delayed Case Progression: The sheer time this takes creates a bottleneck, slowing down the settlement process and capping how many cases a firm can effectively manage.
This old-school approach turns highly skilled legal professionals into data-entry clerks. It pulls their focus from the high-value work they should be doing, like crafting a powerful case narrative or going toe-to-toe with adjusters.
The core problem is that the critical evidence needed to justify a settlement is hidden in unstructured medical data. Searching for it manually is like panning for gold with a teaspoon—you might find something, but you're working way too hard and probably missing the biggest nuggets.
This is exactly where modern technology steps in, turning a labor-intensive chore into a strategic advantage.
The New Way: An AI-Powered Workflow
AI platforms designed for personal injury law, like Ares, completely eliminate this manual bottleneck. Instead of a person reading every single page, the AI scans and understands the entire medical file in minutes. It functions like a super-powered paralegal, instantly finding and pulling out the exact information needed to establish MMI and build a strong case.
This is about more than just speed; it’s about precision and getting the full picture. Efficiently processing medical records is essential for MMI assessments, and solutions like advanced AI-driven medical transcription services can be a huge help in organizing and analyzing these complex files.
With an AI-powered workflow, a firm can:
- Instantly Pinpoint MMI: The technology flags the exact date MMI was declared, the physician who made the call, and the specific report where it’s documented.
- Extract Key Valuations: AI automatically identifies the permanent impairment rating and any recommendations for future medical care—both are absolutely critical for calculating damages.
- Build Data-Driven Demands: By organizing this information logically, the system helps you generate hyper-accurate, evidence-backed demand letters that insurance adjusters take more seriously.
By automating this foundational work, firms can wipe out the risk of oversight, dramatically increase their case capacity, and secure better outcomes for their clients. To see how this works in the real world, check out our complete guide on AI for personal injury lawyers. This shift lets your team stop searching and start strategizing.
Navigating Common MMII Challenges
The road to establishing a final Maximum Medical Improvement date is almost never a straight line. It's one of the most frequently contested milestones in any personal injury case, often tangled up in conflicting medical opinions and frustrating setbacks for your client. Knowing how to handle these bumps is critical to protecting your client’s right to fair compensation.
Probably the most common hurdle you'll face is a premature MMI opinion from a defense-hired Independent Medical Examination (IME). It’s a classic move: the insurance company’s doctor examines your client once and declares them at MMI, sometimes months before their own treating physician agrees. This isn't a medical coincidence; it's a tactic designed to cut off benefits and slash the value of future medical care.
When that IME report lands on your desk, your response has to be fast and built on solid evidence.
Countering a Premature MMI Finding
Your best weapon against a low-ball IME opinion is your client’s own medical history. In most situations, the treating physician’s perspective carries more weight simply because they have the long-term, firsthand view of the patient's entire recovery process, not just a single snapshot in time.
To push back effectively against a premature MMI finding, you'll want to:
- Get a Rebuttal Report: Immediately ask the treating doctor to write a detailed report explaining exactly why they disagree with the IME. This report needs to be specific, pointing to objective evidence of ongoing improvement—like recent gains in physical therapy or a planned surgery that still has curative potential.
- Document the Active Treatment: Make it clear that your client is still actively engaged in—and benefiting from—curative care. If they are making measurable progress or are on the schedule for a procedure, that reality directly contradicts the idea that their condition is permanently stuck.
At its heart, the argument is simple: you can't be at Maximum Medical Improvement if you are, in fact, still medically improving. Documented progress, even if it's slow, is the most powerful evidence you have.
This approach lets you re-center the conversation on your client's actual medical journey, rather than letting a one-off defense exam control the story.
Handling Other Complex MMI Scenarios
Conflicting opinions aren't the only complication. A few other tricky situations can pop up that require a smart, strategic response. Being aware of these possibilities helps you prepare in advance and safeguard your client’s case.
Here are a couple of common, but challenging, scenarios:
- Multiple Injuries, Different MMI Dates: What if your client's shoulder injury stabilizes in a few months, but their complex back injury needs a year or more of treatment? In these cases, the best strategy is usually to wait until all related conditions have reached MMI before you even think about final settlement negotiations. Otherwise, you risk leaving money on the table by undervaluing the total impairment.
- Deterioration After MMI: Sometimes, a client's condition, once deemed "stable," takes a nosedive after the case has settled. It happens. In many states, you can petition to reopen the medical portion of the claim if you can show clear, objective medical evidence that the condition has worsened well beyond what was expected.
Each of these challenges proves that MMI is so much more than a box to check. It's a pivotal, and often hard-fought, milestone that requires diligent documentation and a proactive legal strategy to get right.
Common Questions About Maximum Medical Improvement
Even when you have a good handle on what MMI is, the concept can get tricky as a case develops. It's a major milestone, and it's normal for questions to pop up for both legal teams and their clients. Let's tackle some of the most common ones that arise once an MMI determination enters the picture.
Can My Client Still Get Medical Treatment After Reaching MMI?
Yes, absolutely. This is a huge point of confusion. Reaching MMI doesn't mean your client is cut off from medical care; it just means the type of care changes. We see a shift from curative care to palliative care.
- Curative Care: This is all about healing. Think of surgery to fix a broken bone or physical therapy aimed at getting back lost strength. The goal is improvement, and this is the type of care that stops once MMI is declared.
- Palliative Care: This is about managing the condition for the long haul. It won’t "cure" the injury, but it helps maintain function and reduce pain. Things like regular pain management injections, maintenance physical therapy, or prescriptions to manage chronic symptoms all fall into this category.
Once MMI is established, our job is to calculate the lifetime cost of this necessary palliative care. That figure becomes a cornerstone of the settlement demand.
What Happens if We Don't Agree with the MMI Report?
Disagreements over MMI are incredibly common, especially when the opinion comes from a doctor hired by the defense for an Independent Medical Examination (IME). The good news is you don't have to simply accept it.
An MMI date is not a fact set in stone—it's a medical opinion. And like any opinion, it can be challenged with stronger, more credible evidence.
If you get an MMI finding that feels premature, you have a few moves. The strongest counter is often a detailed report from your client's own treating doctor. They can explain precisely why MMI hasn't been met and detail the progress still being made. You can also depose the IME doctor and poke holes in their conclusion, contrasting their one-off examination with the years of history the treating physician has with your client.
Is an MMI Decision Final?
Not necessarily. While MMI means the condition has plateaued at that moment, it's possible for a claim to be reopened if things change dramatically down the road.
If a client's condition gets significantly worse after the case is closed—far beyond what was medically expected—you might have grounds to reopen the medical part of the claim. This isn't easy; it requires new and compelling medical evidence that proves a major deterioration is directly tied to the original injury. It's a backstop that protects clients whose "stable" condition takes an unforeseen nosedive.
Sifting through thousands of pages of medical records to pinpoint the MMI declaration, impairment ratings, and future care needs is a slow, painstaking process. Ares is designed to find and pull this critical data instantly, helping you build a more powerful demand letter in a fraction of the time. You can stop the manual page-flipping and start settling cases faster. Learn more at Ares Legal AI.